AbstractPurposeThe coronavirus disease 2019 (COVID-19) outbreak has significantly impacted the diagnosis and treatment of breast cancer. Our study investigated the change in diagnosis and treatment of breast cancer with the progress of COVID-19 pandemic.
Materials and MethodsThe study group comprised 6,514 recently diagnosed breast cancer patients between January 1, 2019, and February 28, 2021. The patients were divided into two groups: pre–COVID-19 period (3,182; January 2019 to December 2019) and COVID-19 pandemic period (3,332; January 2020 to February 2021). Clinicopathological information related to the first treatment after breast cancer diagnosis was retrospectively collected and analyzed in the two groups.
ResultsAmong the 6,514 breast cancer patients, 3,182 were in the pre–COVID-19 period and 3,332 were in the COVID-19 pandemic period. According to our evaluation, the least breast cancer diagnosis (21.8%) was seen in the first quarter of 2020. The diagnosis increased gradually except for the fourth quarter in 2020. While early-stage breast cancer was diagnosed 1,601 (48.1%) during the COVID-19 pandemic (p=0.001), the number of surgical treatments increased 4.6% (p < 0.001), and the treatment time was slightly shorter 2 days (p=0.001). The breast cancer subtype distribution was not statistically different between the pre–COVID-19 and COVID-19 period groups.
IntroductionThe response to the global spread of coronavirus disease 2019 (COVID-19) has restructured the health system by urgently identifying and defining health priorities [1]. To minimize the risk to the vulnerable patient population, such as those with cancer, several international associations of healthcare providers recommended cancellation, postponement, or adjustment of non-emergency cancer-related procedures [2,3]. Nevertheless, the COVID-19 outbreak caused worldwide delays in the diagnosis and treatment of cancer patients. Previous studies have also shown that reporting of cancer rates have declined during pandemics in many countries [4–8]. Since the first COVID-19 case on January 20, 2020, in South Korea [9], the pandemic has placed a heavy burden on the Korean healthcare system. However, insufficient data currently exists to understand the effect of COVID-19 on breast cancer diagnosis and treatment in medical institutions that focus on cancer therapy.
Therefore, in this study, we investigated the consequence of the COVID-19 pandemic on breast cancer diagnosis and treatment. For this purpose, differences in clinicopathological factors during the COVID-19 pandemic were evaluated.
Materials and Methods1. Study population and data collectionThe study population consisted of 6,514 patients with newly diagnosed breast cancer. Data were retrospectively collected from patients newly diagnosed between January 2019 and February 2021 at the National Cancer Center, Seoul National University Hospital, and Seoul National University Bundang Hospital. All patients diagnosed with carcinoma in situ during the above-mentioned period, or those diagnosed with breast cancer before January 1, 2019, and received prior treatment at other hospitals and visited the hospital as a new patient, were excluded from the study.
The patients’ clinicopathological characteristics, as recorded in medical records, were analyzed. We divided the patients into two period groups based on their initial diagnosis of breast cancer. The pre–COVID-19 period group consisted of patients diagnosed from January 1, 2019, to December 31, 2019 while the COVID-19 period group was from January 1, 2020, to February 28, 2021. To investigate clinicopathological characteristics, tumor stage was evaluated based on the eighth edition of the American Joint Committee on Cancer. Stage was defined as ‘the clinical stage’ for patients who received neoadjuvant treatment, including chemotherapy, endocrine therapy, or radiotherapy as an initial treatment, and ‘the pathological stage’ for patients who underwent surgery. To assess quarterly differences, the number of diagnoses a, staging distribution for each of the four quarters of 2019 and 2020 were compared.
2. Statistical analysesPatient characteristics were summarized using mean and standard deviation for continuous variables and frequency counts with percentages for categorical variables. For clinical factors, the chi-square test or Fisher’s exact test was used for categorical variables, and the T-test was used for continuous variables for the two groups. The Wilcoxon rank sum test was used to determine the median difference in time duration. To compare the pre–COVID-19 and COVID-19 period groups of each hospital, chi-square test, Fisher’s exact test, t test, or Wilcoxon rank sum test were used. All statistical analyses were performed using R ver. 4.1.2 (R Core Team, Vienna, Austria), and a p-value < 0.05 was considered statistically significant.
Results1. Patterns of diagnosed breast cancerAmong the 6,514 patients, 3,182 cases (48.9%) were newly diagnosed in the pre–COVID-19 period, while 3,332 cases (51.1%) were diagnosed in the COVID-19 pandemic period.
When comparing the two groups during the two periods of 2019 and 2020, the number of breast cancer cases was 3,182 in 2019 and 2,984 cases in 2020. The rate of newly diagnosed breast cancer decreased by 6.2% in 2020 compared with that in 2019. Our analysis shows that the highest diagnosis (26.5%) was seen in the first quarter of 2019 and decreased toward the second half of the year. However, the lowest diagnosis (21.8%) was visible in the first quarter of 2020, which increased gradually with a slight decrease in the fourth quarter. A statistically significant difference (p < 0.001) in the trend of diagnosis per quarter could be observed (Fig. 1).
The quarterly differences between 2019 and 2020 were statistically significant based on the cancer stage distribution. In the second quarter of 2020, when the incidence of COVID-19 was lowest, stage II (38.3% in 2020 vs. 36.9% in 2019) and stage III breast cancer (18.0% in 2020 vs. 14.1% in 2019) reporting increased. Interestingly, as the incidence of COVID-19 gradually increased in the fourth quarter of 2020, stage I breast cancer (54.7% in 2020 vs. 48.0% in 2019) was diagnosed significantly higher than in the same period of 2019 (p < 0.001) (Fig. 2).
We did not observe any statistically significant differences in the number of diagnosed patients based on the region in pre–COVID-19 and the COVID-19 pandemic period groups, even though population density varied between various regions visited by the institution. Gyeonggi/Incheon accounted for the largest proportion, followed by Seoul and Gyeongsang-do (S1 Fig.).
2. Characteristics of breast cancer
Table 1 describes the clinicopathological characteristics of breast cancer patients. The mean age at diagnosis of patients with breast cancer was 53.2±11.1 years. The most common age group was 41–50 years in both groups (34.0% in the COVID-19 pandemic period vs. 34.8% in the pre–COVID-19 period, p=0.556). The detection of breast cancer by screening was higher in the COVID-19 pandemic period than that in the pre–COVID-19 period (54.4% in the COVID-19 pandemic period vs. 51.5% in the pre–COVID-19 period, p=0.001). In terms of the extent of the disease, there were significant statistical differences in the T category and stage grouping. However, the distribution patterns of the stage in the two periods were similar (Table 1).
T1 category was observed to be the most common stage in various T stages with approximately 55% of patients (56.8% in the COVID-19 pandemic period vs. 54.1% in pre–COVID-19, p=0.002), while the N0 category was the most common in N category with approximately 61% patients (62.7% in the COVID-19 pandemic period vs. 59.9% in pre–COVID-19, p=0.071). In the TNM stage, stage I breast cancer was reported most commonly at approximately 46.7% of total patients (48.1% in the COVID-19 pandemic vs. 45.2% in pre–COVID-19, p=0.001). During the COVID-19 pandemic period, a tendency to be diagnosed at an early stage was observed when compared to pre–COVID-19 period (Table 1). We did not observe any statistically significant differences in the distribution pattern of each subtype between the two groups. The hormone receptor (HR)+ subtype was the most common subtype at approximately 73%, followed by the HR−/ human epidermal growth factor receptor 2 (HER)− subtype at approximately 15%, and the HR−/HER2+ subtype at about 11% (Table 1).
3. Differences in treatment of breast cancer
Table 2 presents the observations on the initial treatment for newly diagnosed breast cancer patients. During the COVID-19 pandemic, surgical treatment increased as the first treatment strategy for breast cancer, while the use of chemotherapy or anti-hormonal therapy as the first treatment strategy significantly declined (p < 0.001). The period from the date of diagnosis to the first treatment was averaged at 35 days during the COVID-19 pandemic, seemingly 2 days earlier than the pre–COVID-19 period (p=0.001) (Table 2).
We also performed subgroup analysis by hospitals (Table 3). In hospitals 2 and 3, the number of cases where surgery was used as the first treatment increased significantly during the COVID-19 pandemic period (hospital 2: 81.0% in the COVID-19 pandemic period vs. 64.8% in the pre–COVID-19 period, p < 0.001; hospital 3: 81.7% in the COVID-19 pandemic period vs. 77.2% in the pre–COVID-19 period, p= 0.038). The time from diagnosis to first treatment during the COVID-19 pandemic period was significantly earlier than the pre–COVID-19 period i.e., by an average of 41 days at hospital 1 (5 days earlier, p < 0.001), and 35 days at hospital 2 (2 days earlier, p=0.013).
DiscussionCurrently, the COVID-19 pandemic is a primary health concern in Korea. Since the first outbreak in January 2020, healthcare system changes have been implemented to match the changing COVID-19 variants. The Korean Cancer Association recommended the diagnosis and treatment of breast cancer during the COVID-19 pandemic if a breast cancer screening test was scheduled and if no COVID-19 symptoms were present. Breast cancer screening was majorly postponed if community medical resources were scarce due to the spread of COVID-19 infection. Surgery for cancer treatment was not postponed except in special circumstances and with the recommendation to proceed with the surgery without delay if COVID-19 was in the micro-epidemic stage [10]. The European Society of Medical Oncology and the American Society for Clinical Oncology guidelines recommended that most cancer screening procedures be postponed to preserve healthcare system resources and reduce patient contact with medical institutions unless clinically related cancers are suspected. During the COVID-19 pandemic, telemedicine was used when direct intervention was not required [11,12].
Consequently, opportunities to visit healthcare institutions in Korea decreased as the government proposed social distancing as an important COVID-19 response guideline. According to the 2020 Korean Cancer Registry statistics, the number of newly diagnosed cancer patients in 2020 decreased by 3% compared to 2019, supposedly due to a decrease in the number of cancer screenings during that time.
The number of total cancer cases decreased in March (18.7%) and April (14.4%) 2020 when the first COVID-19 epidemic and high-intensity social distancing were implemented. It increased by 10.7% in June 2020, when the guideline was switched to distancing. A similar pattern has been observed for the other periods as well [13].
One multicenter cohort study in Korea examined the first and second quarters of 2020 and showed that the number of patients diagnosed with breast cancer in 2020 decreased to 9.9%, wherein the period from February to April 2020 and the period from May to July showed 11.2% and 8.8%, respectively. The difference in the initial period was significantly higher [14]. Another retrospective multicenter cohort study reported that the diagnosis and treatment of breast cancer was significantly delayed during the first quarter of 2020 because of quarantine restrictions. Notably, delayed diagnosis and treatment could avoid COVID-19 infection but increase the potential risk to cancer patients [15]. Similarly, our study confirmed the decrease in the number of newly diagnosed breast cancer cases in the first quarter of 2020. However, the number of diagnoses continuously increased in the second half of the year, particularly in the 2nd and 3rd quarters. This was a marked difference from 2019, wherein the diagnosis decreased as the second quarter progressed. We assume that it may be the result of a fear of unknown diseases or the influence of social distancing. COVID-19–related anxiety affected patient’s decision-making. Emotional support to cancer patients can also be seen as an important factor during the COVID-19 pandemic [16].
Previous studies have reported that many cancers advanced during the COVID-19 pandemic. In a study from Turkey, there was a significant increase in newly diagnosed stage IV breast cancer during the COVID-19 pandemic [17]. Another study from the United Kingdom reported that breast cancer patients presented more aggressive patterns, including node positivity and advanced stage, in 2020 than in 2019 [18]. Interestingly, our study showed results that were different from previously published studies. During the COVID-19 pandemic, early-stage cancer reporting showed an increase; as a result, surgical treatment was performed first rather than neoadjuvant treatment. This is different from previous studies, possibly, because our institutions focus on cancer treatment, and cancer patients may have easy access at an early stage. We have shown that those who do not have COVID-19 were actively screened for cancer even during the coronavirus pandemic.
COVID-19 vaccination [19] was introduced in Korea in February 2021 with a high vaccination rate of approximately 87%. After the 5th peak COVID-19 wave, we are currently in a COVID-19 pandemic era in which Omicron (B.1.1.529) is dominating. Compared to the pandemic beginning, the severity of COVID-19 has been greatly alleviated, and the medical system and response policies have constantly been changing. Still, changes in the COVID-19 status could have a significant impact on the diagnosis and treatment of breast cancer in the future.
The strength of the study lies in its comparison of changes in the fourth quarter after the COVID-19 pandemic, unlike previous studies. Previous studies compared the initial state in Korea [14,20]; therefore, the subsequent pattern could not be identified. Furthermore, our study included a large number of participants and identified the distribution and characteristics of breast cancers during the COVID-19 pandemic. When the diagnosis of breast cancer decreased and recovered, the cancer was relatively advanced at the beginning; however, when the diagnosis service was restored, relatively early cancer diagnosis increased, confirming the importance of screening for cancer. In addition, we have confirmed that an event such as an epidemic/pandemic greatly influences breast cancer diagnosis.
Our study did possess some limitations. It was a retrospective study. Since we analyzed data based on medical records, data on some clinical factors, such as comorbidity and other family histories of the subject, were incomplete. In addition, the symptoms of cancer, mostly subjective, cannot be compared by subdividing. We did not analyze the diagnostic forms of breast cancer after vaccination. Changes in patterns after vaccination require further analysis. Despite these limitations, this analysis is useful for understanding the influence of COVID-19 on patients’ treatment decisions and emerging acute healthcare issues.
In conclusion, COVID-19 temporarily affected the diagnosis and treatment of breast cancer during the early stages of the COVID-19 outbreak; however, later diagnosis and treatment were stabilized by the quarantine system and treatment recommendations.
Electronic Supplementary MaterialSupplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
NotesEthical Statement This study was approved by the Institutional Review Board of the National Cancer Center (IRB number: NCC2021-0258) and conducted in accordance with the tenets of the Declaration of Helsinki. The requirement for informed consent was waived because the study was a retrospective medical record review. Author Contributions Conceived and designed the analysis: Lee EG, Kim EK, Jung SY, Moon HG. Collected the data: Lee EG, Han Y, Koh HW. Contributed data or analysis tools: Lee DE. Performed the analysis: Lee DE. Wrote the paper: Lee EG, Jung SY. Writing - review and editing: Lee EG, Lee DE, Moon HG, Han Y, Ko HW, Kim EK, Jung SY. Funding acquisition: Jung SY. Supervision: Kim EK, Jung SY. Fig. 1Number of newly diagnosed breast cancer patients after onset of coronavirus disease 2019 (COVID-19) at three hospitals. 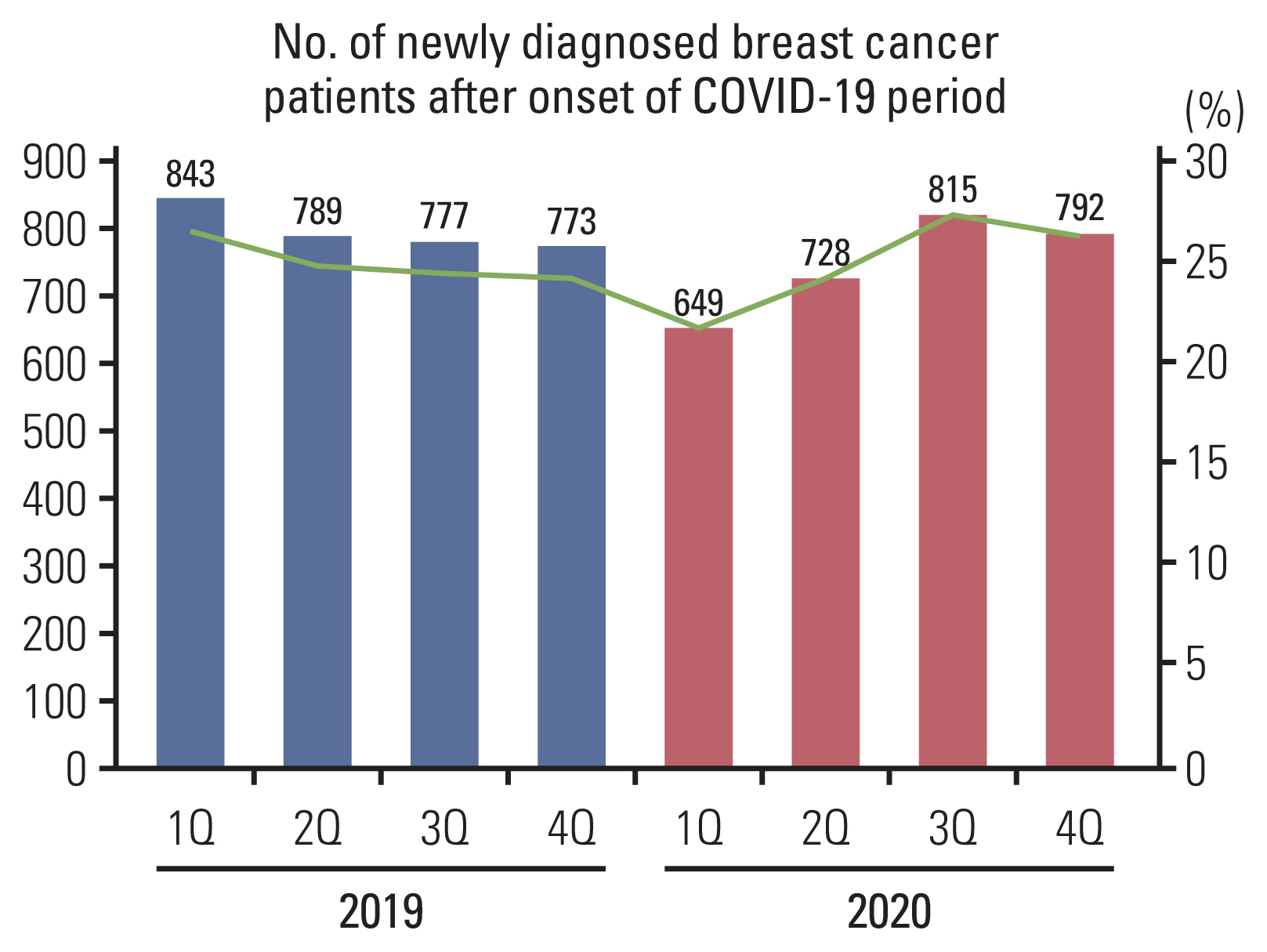
Table 1Baseline characteristics of the population
Table 2First treatment of the population
Table 3Comparison of cancer patients’ characteristics between three hospitals in the two groups
References1. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382:2049–55.
3. Hanna TP, Evans GA, Booth CM. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17:268–70.
4. De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared with the 2018–2019: an audit study from cellular pathology. J Clin Pathol. 2021;74:187–9.
5. Jacob L, Loosen SH, Kalder M, Luedde T, Roderburg C, Kostev K. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers (Basel). 2021;13:408.
6. Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;3:e2017267.
7. Mahase E. COVID-19: urgent cancer referrals fall by 60%, showing “brutal” impact of pandemic. BMJ. 2020;369:m2386.
8. Zadnik V, Mihor A, Tomsic S, Zagar T, Bric N, Lokar K, et al. Impact of COVID-19 on cancer diagnosis and management in Slovenia: preliminary results. Radiol Oncol. 2020;54:329–34.
9. Dighe A, Cattarino L, Cuomo-Dannenburg G, Skarp J, Imai N, Bhatia S, et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. 2020;18:321.
10. Lee JB, Jung M, Kim JH, Kim BH, Kim Y, Kim YS, et al. Guidelines for cancer care during the COVID-19 pandemic in South Korea. Cancer Res Treat. 2021;53:323–9.
11. de Azambuja E, Trapani D, Loibl S, Delaloge S, Senkus E, Criscitiello C, et al. ESMO management and treatment adapted recommendations in the COVID-19 era: Breast Cancer. ESMO Open. 2020;5:e000793.
12. American Society of Clinical Oncology. Cancer screening, diagnosis, staging and surveillance [Internet]. Alexandria, VA: American Society of Clinical Oncology; 2020 [cited 2023 Jan 18]. Available from: https://www.asco.org/covid-resources/patient-care-info/cancer-screening-diagnosis-staging
13. Korea Central Cancer Registry. 2020 Cancer statistics [Internet]. Goyang: National Cancer Center; 2022 [cited 2023 Jan 18]. Available from: https://ncc.re.kr/cancerStatsView.ncc?bbsnum=618&searchKey=total&searchValue=&pageNum=1
14. Kang YJ, Baek JM, Kim YS, Jeon YW, Yoo TK, Rhu J, et al. Impact of the COVID-19 pandemic on the diagnosis and surgery of breast cancer: a multi-Institutional study. J Breast Cancer. 2021;24:491–503.
15. Li J, Wang H, Geng C, Liu Z, Lin Y, Nie J, et al. Suboptimal declines and delays in early breast cancer treatment after COVID-19 quarantine restrictions in China: a national survey of 8397 patients in the first quarter of 2020. EClinicalMedicine. 2020;26:100503.
16. Vanni G, Materazzo M, Pellicciaro M, Ingallinella S, Rho M, Santori F, et al. Breast cancer and COVID-19: the effect of fear on patients’ decision-making process. In Vivo. 2020;34:1651–9.
17. Ilgun AS, Ozmen V. The impact of the COVID-19 pandemic on breast cancer patients. Eur J Breast Health. 2022;18:85–90.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||