AbstractBreast metastases from an extramammary primary tumor are very rare and the prognosis for such patients is generally poor. We report here on a case of a 42-year-old female with metastasis of non-small cell lung cancer to the breast, and she is now being followed up on an outpatient basis. In 2004, she presented with a solitary pulmonary nodule in the left lung, and this lesion had been noted to have gradually increased in size over time. The final pathological diagnosis was adenocarcinoma, and the diagnosis was made by performing percutaneous needle aspiration and lobectomy of the left upper lobe. Adjuvant chemotherapy and radiotherapy were given. Unfortunately, a nodule in the left breast was noted three years later, and metastatic non-small-cell lung cancer to the breast was diagnosed by excisional biopsy. Making the correct diagnosis to distinguish a primary breast carcinoma from a metastatic one is important, because the therapeutic plan and outcome for these two types of cancer are quite different.
IntroductionNon-small cell lung cancer (NSCLC) accounts for approximately 75% to 80% of all the types of lung cancer, and it is the leading cause of cancer-related deaths worldwide (1). While small cell lung cancer can metastasize to nearly all the organs, metastasis from NSCLC is most commonly seen in the liver, adrenal glands, bone, brain, kidney and abdominal lymph nodes.
Breast metastases from an extramammary primary tumor, including NSCLC, are very rarely reported, with the incidence being 0.5% to 3% of all the breast malignancies. The prognosis of these patients is poor. We report here on a case of a 42-year-old woman with metastasis to the breast from adenocarcinoma of the lung.
Case ReportA 42-year-old female presented in November 2001 with a solitary pulmonary nodule in the left lung, and the nodule had gradually increased in size since initially detected 1 year before. Chest computed tomography (CT) was done, which revealed a 2 cm sized spiculated nodule in the left upper lobe (Fig. 1). Percutaneous needle aspiration was performed, and the histological diagnosis was adenocarcinoma (Fig. 2).
The stage of disease was T2N1M0, stage IIB. The patient underwent curative lobectomy of the left upper lobe, and she was started on six cycles of adjuvant chemotherapy (etoposide 75 mg/m2 and cisplatin 75 mg/m2), followed by postoperative radiation therapy (5,400 cGy in 30 fractions) to the left hilar and mediastinual lymphatics. The patient was asymptomatic for the next three years with no evidence of recurrence. In October 2004, a follow-up chest radiograph and chest CT showed suspicious small nodules with enhancement in the left breast. Breast ultrasonography (USG) showed two oval and round shaped homogeneous hypoechoic lesions (category 4/5), which were 1.2 cm and 0.8 cm in diameter over the 12 o'clock and 1 o'clock directions of the left breast, respectively (Fig. 3). An excisional biopsy was conducted, which revealed well-differentiated adenocarcinoma.
The tumor cells were positive for thyroid transcription factor-1 (TTF-1) and E-cadherin, and were negative for estrogen receptors (ER) and progesterone receptors (PR), p53 and Her2 on the immunohistochemical staining (Fig. 4). The histologic features were consistent with those of the previous biopsy specimen of her lung cancer, suggesting the new lesions were metastatic breast cancer from the lung, rather than primary carcinoma of the breast. From November 22, 2004 to January 15, 2005, the patient subsequently received four cycles of chemotherapy with docetaxel (75 mg/m2) and cisplatin (75 mg/m2). The patient was asymptomatic with no evidence of recurrence until November 21, 2007, and then the follow-up chest CT showed suspicious small nodules with enhancement in the retroareolar portion of the left breast operation site. Breast USG and positron emission tomography (PET)-CT were done. The nodules were strongly suspicious of being metastatic nodules. Fine-needle biopsy and simple mastectomy were performed, and the histopathologic evaluation was consistent with metastatic adenocarcinoma from the lung, which implied metachronous metastasis to the breast. The immunohistochemical staining was negative for estrogen and progesterone receptors, but it was positive for TTF-1, E-cadherin and CK7.
We thought that the breast nodules originated from the lung. From February 13, 2008 to May 22, 2008, the patient received four cycles of chemotherapy with gemcitabine (1,000 mg/m2) and cisplatin (75 mg/m2). The patient was re-examined with chest CT and breast USG in June, 2008. There was no evidence of local recurrence on the breast USG, but the chest CT revealed a 1 cm sized nodule in the right middle lobe (RML). Wedge resection via explo-thoracotomy was performed, and the histopathologic diagnosis was interstitial inflammation with fibrosis. The patient is currently being followed-up on an outpatient basis with no evidence of disease.
DiscussionLung cancer continues to be a leading cause of cancer-related deaths in humans, with adenocarcinoma being the most frequent histological subtype. The reported frequency of metastasis at the time of diagnosis of NSCLC has varied from 11% to 36%, and the common metastatic sites include the liver, adrenal gland, brain, bone, kidney and abdominal lymph nodes (2,3). The other unusual metastatic sites that have been reported are the stomach, pancreas, small bowel, arteriovenous hemangioma, choroid plexus, muscle, umbilicus and penis.
NSCLC with metastasis to the breast has rarely been reported in the medical literature. Most of the primary lung cancers metastasizing to the breast are adenocarcinoma, while other types of lung carcinoma, including small cell carcinoma, are relatively rare. Breast involvement by metastatic solid tumors in uncommon (4) due to the large areas of fibrous tissue and relatively poor blood supply in the breast (5). In female patients, the most common primary metastatic sites/tumors are the contralateral breast, lymphoma, leukemia, malignant melanoma and rhabdomyosarcoma (6-8). The outcomes of patients with breast metastases are poor, and 80% of these patients die within 1 year of presentation (9). However, in our case, the patient shows no-evidence of disease, and she is currently being followed-up on an outpatient basis after the diagnosis of metastatic cancer to the breast in October 2004.
Differentiation between primary and metastatic cancer to the breast is very important for the therapeutic plan. Metastatic malignancy to the breast generally presents as freely mobile, well-circumscribed, firm and round masses without skin change, and so distinguishing between benign and malignant breast lesions is difficult. Mammography is a useful diagnostic tool for the differential diagnosis of primary breast cancer and metastatic cancer to the breast. The typical mammographic findings of metastatic cancer to the breast are generally a well-defined, dense mass (10) without the characteristics of primary breast carcinoma such as distortion of the adjacent architecture or microcalcification (10,11). Multiple masses and the absence of hormone receptors are favorable presentations for the metastatic lesions of the breast.
Although mammography, breast USG and CT scanning can provide some information to distinguish primary breast cancer from metastatic disease, conducting a pathologic examination with the fine-needle aspiration cytology is essential for accurate diagnosis (9). Excisional or core biopsy is usually needed for the pathological confirmation. The immunohistochemical features may need to be assessed to additionally confirm the diagnosis. Immunoreactivity for TTF-1 is crucial for verifying that a malignancy originates from the lung. TTF-1 is the homeodomain-containing nuclear transcription protein of the NKx2 gene, and the NKx2 gene is a member of the family of homeobox-containing genes in Drosophila. TTF-1 is expressed in the epithelial cells of the thyroid gland and lung, and also in the adenocarcinomas that are derived from these cells (12). TTF-1 has been shown to be a sensitive and highly specific marker for adenocarcinomas, of a pulmonary origin, in tissue biopsies and cytological preparations. TTF-1 is expressed in 62% to 88% of all the primary lung adenocarcinomas, but it is expressed in less than 1% of the adenocarcinomas of a non-pulmonary origin (13). Several studies have also revealed that TTF-1 was not specific for, and is rarely positive in, primary breast cancer (14). Metastatic cancer to the breast is very rare, but it is important to consider this possibility to ensure the appropriate management, and particularly in smokers with a previous diagnosis of malignancy.
A careful clinical history of a concurrent or previous diagnosis of malignancy combined with the clinical examination, radiological assessment and cytological evaluation is needed to diagnose breast adenocarcinoma that has metastasized from the lung.
References1. Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics, 2001. CA Cancer J Clin. 2001;51:15–36. PMID: 11577478
2. Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer. 1950;3:74–85. PMID: 15405683
3. Quint LE, Tummala S, Brisson LJ, Francis IR, Krupnick AS, Kazerooni EA, et al. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg. 1996;62:246–250. PMID: 8678651
4. Rosen PP. In : Rosen PP, editor. Metastases in the breast from nonmammary malignant neoplasm. Rosen's pathology of the breast. 2001. 2nd edPhiladelphia: Lippincott Williams & Wilkins; p. 689–707.
5. Yeh CN, Lin CH, Chen MF. Clinical and ultrasonographic characteristics of breast metastases from extramammary malignancies. Am Surg. 2004;70:287–290. PMID: 15098776
6. Toombs BD, Kalisher L. Metastatic disease to the breast: clinical, pathologic, and radiographic features. AJR Am J Roentgenol. 1977;129:673–676. PMID: 409241
7. Sheen-Chen SM, Liu YW, Eng HL, Huang CC, Ko SF. Metastatic malignant pleural mesothelioma to the breast. South Med J. 2006;99:1395–1397. PMID: 17233200
8. Sheen-Chen SM, Eng HL, Ko SF. Metastatic rhabdomyosarcoma to the breast. Anticancer Res. 2005;25(1B):527–529. PMID: 15816623
9. Sneige N, Zachariah S, Fanning TV, Dekmezian RH, Ordóñez NG. Fine-needle aspiration cytology of metastatic neoplasms in the breast. Am J Clin Pathol. 1989;92:27–35. PMID: 2750705
10. Chaignaud B, Hall TJ, Powers C, Subramony C, Scott-Conner CE. Diagnosis and natural history of extramammary tumors metastatic to the breast. J Am Coll Surg. 1994;179:49–53. PMID: 8019724
11. Bohman LG, Bassett LW, Gold RH, Voet R. Breast metastases from extramammary malignancies. Radiology. 1982;144:309–312. PMID: 7089284
12. Pelosi G, Fraggetta F, Pasini F, Maisonneuve P, Sonzogni A, Iannucci A, et al. Immunoreactivity for thyroid transcription factor-1 in stage I non-small cell carcinomas of the lung. Am J Surg Pathol. 2001;25:363–372. PMID: 11224607
13. Ordóñez NG. Thyroid transcription factor-1 is a marker of lung and thyroid carcinomas. Adv Anat Pathol. 2000;7:123–127. PMID: 10721419
14. Harlamert HA, Mira J, Bejarano PA, Baughman RP, Miller MA, Whitsett JA, et al. Thyroid transcription factor-1 and cytokeratins 7 and 20 in pulmonary and breast carcinoma. Acta Cytol. 1998;42:1382–1388. PMID: 9850647
Fig. 1Chest CT shows a slender nodule (2 cm in length) in the left upper lobe (the anterior apical segment). 
Fig. 2The microscopic findings of the lung biopsy show adenocarcinoma (the bronchial-alveolar type). 
Fig. 3(A) Chest CT reveals suspicious small nodules with enhancement in the left breast. (B) Breast ultrasonography showed two oval or round shaped homogeneous hypoechoic lesions (category 4/5). The two nodules were 1.2 cm in diameter over the 12 o'clock direction and 0.8 cm in diameter over the 1 o'clock direction of the left breast. 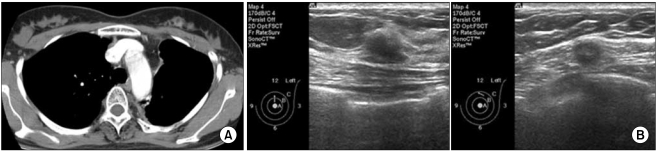
Fig. 4(A) Breast biopsy shows a well differentiated adenocarcinoma (H&E, ×400). (B) Immunohistochemical staining for thyroid transcription factor-1 (TTF-1) in the adenocarcinoma of the breast. (C) The immunohistochemical staining is negative for estrogen receptor (ER) and progesteron receptor (PR) in the adenocarcinoma of the breast. 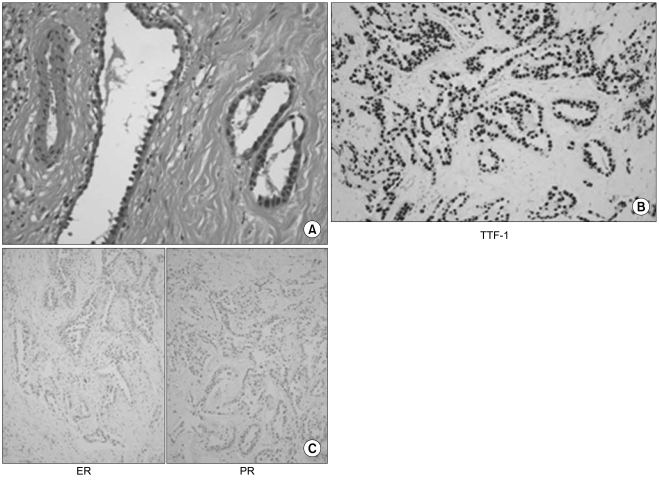
|
|
|||||||||||||||||||||||||||||||||||||||||||