A Phase II Study of Modified FOLFOX4 for Colorectal Cancer Patients with Peritoneal Carcinomatosis
Article information
Abstract
Purpose
Peritoneal carcinomatosis (PC) of colorectal cancer (CRC) is common and is the second most common cause of death. Clinical studies regarding chemotherapy for CRC with PC have been classically rather limited in scope. We evaluated the efficacy of modified oxaliplatin, leucovorin, and fluorouracil (m-FOLFOX4) regimen for PC of CRC origin.
Materials and Methods
CRC patients with PC were treated with cycles of oxaliplatin at 85 mg/m2 on day 1, leucovorin 20 mg/m2 followed by 5-fluorouracil (5-FU) via a 400 mg/m2 bolus and a 22 hours continuous infusion of 600 mg/m2 5-FU on days 1-2 at 2-week intervals.
Results
Forty patients participated in this study. Median age was 55 years. Thirty-two patients (80.0%) received previous operation, and 60.0% of PC occurred synchronously. Thirty-five patients (87.5%) were assessable and exhibited measurable lesions. Two patients (5.7%) demonstrated complete response and five patients (14.3%) showed partial response. The median time to progression was 4.4 months (95% confidence interval, 2.5 to 6.3 months), the median overall survival time was 21.5 months (95% confidence interval, 17.2 to 25.7 months). There was no treatment related death. Presence of liver metastasis (p=0.022), performance status (p=0.039), and carcinoembryonic antigen level (p=0.016) were related to the time to progression. Patients with low carcinoembryonic antigen level (37.2 months vs. 15.6 months, p=0.001) or good performance status (22.5 months vs. 6.8 months, p=0.040) showed better overall survival.
Conclusion
The m-FOLFOX4 regimen was determined to be effective for CRC patients with PC.
Introduction
Colorectal cancer (CRC) is the fourth most frequent cause of cancer-specific death in Korea [1]. Peritoneal carcinomatosis (PC) of colorectal origin is common and is the second-most frequent cause of death in CRC after metastatic disease to the liver. PC may cause serious complications, including intestinal obstruction, massive ascites, and hydronephrosis, which are associated clinically with abdominal pain and fullness, vomiting, constipation, malnutrition, and renal dysfunction. The incidence of PC during potentially curative surgery for primary CRC was reported as 3% to 28%, which may be explained by differences in methods to detect cancer cells [2]. Mechanisms of PC development are still controversial, and include spreading of free cancer cells due to serosal involvement of the primary tumor, lymphatic and or venous dissemination of malignant cells, and implantation of free cancer cells due to the presence of adherence molecules [3]. It would appear that the mechanisms responsible are multifactorial. Three principal studies [4-6] showed the natural history of PC from CRC, and confirmed a poor prognosis with a median survival ranging between 6 and 8 months and no 5-year survivors. Because of its poor prognosis, PC from CRC has previously been considered a preterminal condition suitable only for palliative treatment.
Sugarbaker et al. introduced cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) as anew innovative therapeutic option for selected patients with PC to improve long-term survival for selected patients [7]. Recently, it was reported that a 5-year survival rate of 51% and median survival of 63 months in patients with limited PC treated with oxaliplatin-based HIPEC [8]. While the initial results utilizing these techniques have been promising, caution must be exercised before recommending them as first-line treatment modalities. In the literature, morbidity and mortality rates after CRS and HIPEC range from 25% to 41% and from 0% to 8%, respectively [9]. Furthermore, the majority of patients with PC from CRC present with an unresectable disease at the time of diagnosis, therefore CRS and HIPEC is not indicated for those patients.
In the past two decades, chemotherapeutic treatment of patients with metastatic CRC has rapidly evolved. The FOLFOX regimen of oxaliplatin and infused fluorouracil (5-FU) plus leucovorin (LV) is active and comparatively safe. It is considered as a standard therapy for patients with advanced CRC [10]. We previously reported a median time to progression (TTP) of 8.7 months, response rate of 45%, and median survival time of 19.5 months for metastatic CRC using modified FOLFOX4 (m-FOLFOX4) regimen [11]. Nonetheless, the patient cohorts with Stage IV disease in these trials failed to include patients with PC. The difficulties of including these patients are a result of the inability to image sub-centimeter peritoneal lesions and assess tumor response on the Response Evaluation Criteria in Solid Tumors (RECIST) criteria. Thus, only a few reports are currently available regarding the efficacy of systemic chemotherapy against PC.
The studies investigating the prognosis of isolated PC treated with chemotherapy showed median survival lasting from 5.2 to 12.6 months [4-6, 12]. However, in these studies, only 5-FU-based chemotherapy was administered without modern drugs like oxaliplatin or irinotecan.
The aim of this study was to evaluate the safety and efficacy of oxaliplatin with low dose LV and bolus and continuous infusion 5-FU (m-FOLFOX4) for the treatment of patients with CRC with PC.
Materials and Methods
1. Patients
Patients were required to have a histologically-confirmed adenocarcinoma arising in the colon or rectum. All patients had PC with or without measurable lesions, a performance status ≤2 according to the Eastern Cooperative Oncology Group (ECOG) scale, adequate bone marrow and renal function, and age between 18 and 75 years. Exclusion criteria included the presence of central nervous system metastases, serious or uncontrolled concurrent medical illness, and a history of other malignancies. Patients with synchronous disease were diagnosed at the time of presentation with CRC, either on routine staging, computed tomography (CT), or at laparotomy. Patients with metachronous carcinomatosis were deemed to be clear of peritoneal disease at the initial curative colorectal resection, but subsequently became symptomatic on follow-up and were diagnosed with peritoneal metastases on CT. The study was approved by the local ethics committee, and informed consent was obtained from all patients before study entry.
2. Treatment protocols and dose modification
On day 1, oxaliplatin (85 mg/m2) was administered by intravenous (IV) infusion in 500 mL of normal saline or dextrose over 2 hours IV infusion. On days 1 and 2, LV (20 mg/m2) was administered as an IV bolus, immediately followed by 5-FU (400 mg/m2) given as a 10 minute IV bolus, followed by 5-FU (600 mg/m2) as a continuous 22 hours infusion, with a light shield. Dose modifications of oxaliplatin or 5-FU were made for hematologic, gastrointestinal, or neurologic toxicities on the basis of the most severe grade of toxicity that had occurred during the previous cycle. Treatment could be delayed for up to 2 weeks if symptomatic toxicity persisted, or if the absolute number of neutrophils was lower than 1,500/µL; platelets count was lower than 100,000/µL. The 5-FU dose was reduced by 25% for subsequent courses after occurrence of National Cancer Institute Common Toxicity Criteria (NCI-CTC) grade 3 diarrhea, stomatitis, or dermatitis. The dose of oxaliplatin was reduced by 25% in subsequent cycles if there was persistent paresthesia between cycles or paresthesia with functional impairment lasting more than 7 days. Treatment was continued until there were signs of disease progression, development of unacceptable toxic effects, or the refusal by patient of further treatment.
3. Pretreatment and follow-up evaluation
Before each treatment courses, a physical examination, routine hematologic studies, blood chemistry, and chest X-ray were performed. The serum carcinoembyromic antigen (CEA) levels were determined after each cycle. CT scans to define the extent and the response of the disease were performed after 4 cycles of chemotherapy, or sooner if there was evidence of any clinical deterioration. Patients were assessed before starting each 2-week cycle using the NCI-CTC, except in the case of neurotoxicity. For the neurotoxicity, an oxaliplatin-specific 3-grade scale was used: grade 1, paresthesias or dysesthesias of short duration, but resolving before the next dosing; grade 2, paresthesias persisting between doses (2 weeks); and grade 3, paresthesias interfering with function.
4. Assessment of response
Responses were evaluated using RECIST criteria [13]. Complete response (CR) was defined as the disappearance of all evidence of disease and the normalization of tumor markers for at least 2 weeks. Partial response (PR) was defined as ≥30% reduction in uni-dimensional tumor measurements, without the appearance of any new lesions or the progression of any existing lesion. Progressive disease (PD) was defined as any of the following: 20% increase in the sum of the products of all measurable lesions, appearance of any new lesion, or reappearance of any lesion that had previously disappeared. Stable disease (SD) was defined as a tumor response not fulfilling the criteria for CR, PR, or PD.
The dose-intensity (mg/m2/wk) was calculated as the total cumulative dose divided by the duration of dosing. The relative dose-intensity (RDI) was calculated as the dose-intensity divided by the planned dose-intensity, multiplied by 100. The planned dose-intensities, expressed as milligrams per square meter per week, were 1,000 for 5-FU and 42.5 for oxaliplatin.
5. Statistical methods
This trial was designed to detect a response rate of 30%, as compared with the minimal, clinically meaningful response rate of 10%. A two-stage optimal design, as previously proposed, was adopted [14], with a statistical power of 80% for hypothesis acceptance and 5% significance for hypothesis rejection. Allowing for a follow-up loss rate of up to 10%, the total sample size required was 35 patients with measurable disease. Categorical variables in the two groups were compared by the χ2 test or Fisher's exact test. p-values<0.05 were considered statistically significant and all p-values correspond to two-sided significance tests. The primary study endpoint was from the time of diagnosis of PC to the time of death. TTP and overall survival (OS) were calculated via the Kaplan-Meier method. TTP was calculated from the date therapy was initiated to the date of disease progression, death, or final follow-up. OS was calculated from the date therapy was initiated to the date of death or final follow-up. The log-rank test was employed to compare distributions. Due to the small number of patients the performance of a multivariate analysis was not considered to be useful. All data were analyzed with SPSS ver. 18.0 (SPSS Inc., Chicago, IL).
Results
1. Patient characteristics
Beginning in January 2002, 40 patients were assigned for treatment at the Department of Internal Medicine at the Dong-A University Medical Center in Busan, Korea. The male to female ratio in this study was 20 : 20, and the median patient age was 55 years (range, 28 to 75 years). PC was present at time of resection of the primary tumors in 24 patients, and it was diagnosed as recurrent disease in 16 patients with an average disease-free interval of 16.5 months (range, 0 to 33 months). Thirty-two patients (80.0%) received a previous operation, and ascites was present at diagnosis of the primary tumor in 20.0% of patients. Thirty-two patients (80.0%) were judged to have an ECOG performance status of 0-1. Thirty-five patients (87.5%) initially presented with at least one measurable lesion. The most frequent site of involvement was abdominal lymph node (50.0%), followed by the liver (32.5%), ovary (20.0%), and lung (15.0%).
2. Response and toxicities
Thirty-five patients were assessed for response with measurable lesions. Two patients achieved CR (5.7%), 5 patients showed PR (14.3%), 17 patients (48.6%) had SD, and 11 patients (31.4%) manifested PD. Patients who had liver metastasis displayed a better response rate (31.8% vs. 0%, p=0.031). Patients with low serum CEA also showed better response (57.1% vs. 10.7%, p=0.018). Forty patients received a total of 294 treatment cycles. The median number of cycles administered was 6 cycles (range, 2 to 12 cycles). Dose reductions were required on nine occasions. The dose intensities of oxaliplatin and 5-FU were 40.6 mg/m2/wk and 976.5 mg/m2/wk, and the RDIs of oxaliplatin and 5-FU were 95.5 and 97.7%.
Toxicities observed during the treatment are as follows. Grade 1 or 2 anemia (50.0%) was the most frequently observed hematological toxicity, and grade 3 or 4 neutropenia was detected in 15.5% of the cycles. Nine cycles (3.1%) of febrile neutropenia were recorded, and grade 2 or 3 nausea/vomiting were noted in 6 patients (15.0%). Grades 1 and 2 neuropathy was observed in 6 patients (15.0%). However, no patients experienced neuropathy of grade 3 or more. No treatment related deaths occurred in this study.
3. Survival
The median follow up duration was 22.9 months (range, 2.4 to 71.8 months). The median TTP was 4.4 months (95% confidence interval [CI], 2.5 to 6.3 months), and the median OS duration was 21.5 months (95% CI, 17.2 to 25.7 months). TTP and OS were evaluated via Kaplan-Meier analysis, as shown in Figs. 1 and 2. Several potential prognostic factors were analyzed for survival differences: ECOG performance status, disease-free interval, presence of liver, lung metastases and ascites, and serum CEA level (Table 1). Presence of liver metastasis (p=0.022), performance status (p=0.039), and CEA level (p=0.016) were related to the TTP. Patients with low CEA level (37.2 months vs. 15.6 months, p=0.001), or good performance status (22.5 months vs. 6.8 months, p=0.040) showed better OS. No other intrinsic patient and tumor characteristics involved in the univariate analysis seemed to have a clear influence on OS. Given these results, performing a multivariate analysis would not have been useful.
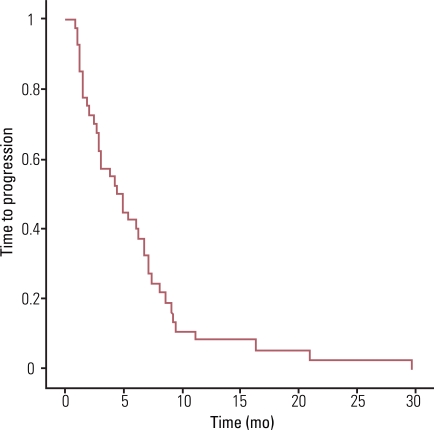
Time to progression curve. Median time to progression was 4.4 months (95% confidence interval, 2.5 to 6.3 mo).
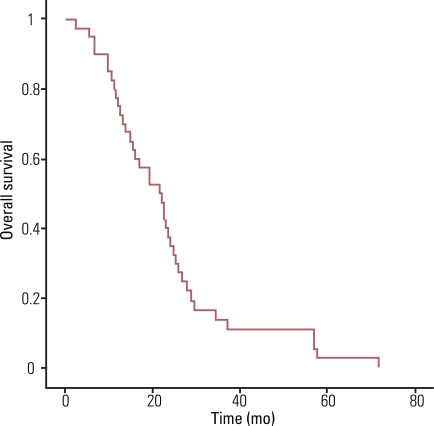
Overall survival curve. Median overall survival was 21.5 months (95% confidence interval, 17.2 to 25.7 mo).
Discussion
A subgroup of patients presenting with isolated intraperitoneal metastases without evidence of systemic disease contributed to the development of new locoregional treatment strategies consisting of CRS and HIPEC. In selected patients, this aggressive surgical approach results in a significant survival benefit [9]. Unfortunately, only a small and highly selected group of patients with limited disease confined to the peritoneal cavity is eligible for this treatment, therefore most patients suffering from PC are dependent on palliative systemic chemotherapy.
Chu et al. [4] reported on a series of 100 patients with PC of nongynecologic tumors, among whom 45 patients had CRC. In the patients with CRC, of whom the majority was treated with 5-FU and LV, median survival was 6 months. Shorter disease-free interval, presence of lung metastases, and presence of ascites correlated significantly with decreased survival [4]. A multi-centre prospective study (EVOCAPE1) reported on 118 patients with PC from CRC with a median survival of 5.2 months [13]. Only the extent of PC was significantly correlated to survival. Synchronous PC, T stage, lymph node involvement, tumor differentiation, presence of ascites, and presence of liver metastases did not have a statistically significant influence on prognosis. In a retrospective analysis of 3019 patients with CRC, 349 (13%) of the patients presented with PC, 214 patients (7%) had synchronous PC at the time of resection of the primary tumor, whereas another 135 patients (4.5%) developed metachronous carcinomatosis [6]. The 349 patients who presented with PC had a median survival of 7 months. In the PC group, a significantly higher proportion of primary tumors had advanced disease stage at diagnosis. Furthermore, extent of PC disease and T stage were identified as predictors of survival for synchronous PC. In a phase III randomized controlled trial of 50 patients who were treated with systemic chemotherapy and palliative surgery obtained an overall median survival of 12.6 months with a 2-year survival rate of 18% and a median time to disease progression of 7.6 months [12].
Although the favorable effect of modern chemotherapy treatment on the survival of patients with metastatic disease in general has been well described, it remains unclear whether these systemic therapies have the same beneficial impact on the outcomes of the subset of patients diagnosed with PC. Despite increasing usage of palliative chemotherapy and availability of new agents, population-based survival of patients with PC has not improved until very recently. Response to palliative chemotherapy in PC should be evaluated separately from hematogenous metastases. At the present time, there is only one published study that outlines the impact of the new systemic therapy regimens when given to CRC patients with PC [15]. The study reported a median survival of 5 months (95% CI, 3 to 7 months) for patients who had no chemotherapy, 11 months (95% CI, 6 to 9 months) for patients treated with 5-FU/LV, and 12 months (95% CI, 4 to 20 months) for patients treated with oxaliplatin/irinotecan-based chemotherapy. In our study, we observed that the median OS was 21.5 months, compatible with a previous study [10]. To our knowledge, such high median OS has never been reported for patients with CRC with PC in the literature, and may be due to the facts that most patients had good performance status and the number of metastasis was less than three. This is the highest median survival that can currently be obtained with systemic treatment and without recent targeted therapies. We also showed that good performance status and low level of CEA were related to better survival. However, none of the above-mentioned adverse predictive factors in other studies had a statistically significant influence on outcome.
Conclusion
Our data demonstrates that m-FOLFOX4 is likely to be beneficial in patients with PC of CRC, especially the patients with good performance status and low CEA. The results of this study support the rationale for palliative treatment with the best available systemic chemotherapy schedules for patients with PC who do not meet the inclusion criteria for CRS and HIPEC. Future research should focus on developing the optimal combination of palliative chemotherapy regimens for patients suffering from PC of CRC.
Acknowledgments
This paper was supported by the Dong-A University Research Fund.
Notes
Conflict of interest relevant to this article was not reported.
