Marked Reduction in the Risk of Dementia in Patients with Breast Cancer: A Nationwide Population-Based Cohort Study
Article information
Abstract
Purpose
An inverse relationship between cancer and neurodegenerative disease, which presents the possibility of a reduced risk of dementia in cancer patients, has been suggested previously. However, a nationwide longitudinal population-based study of specific types of cancer with due consideration of treatment effects has not been conducted.
Materials and Methods
This nationwide population-based cohort study used data obtained in a 12-year period (January 2007–December 2018) in the Korean National Health Insurance claims database. All female breast cancer patients (age ≥ 50 years) diagnosed between 2009 and 2010 were included after excluding those with physician visits for any cancer during a 2-year period (2007–2008). Patients with senile cataract constituted the control group. The main study outcome was the risk of developing dementia.
Results
From a total of 90,396 and 85,906 patients with breast cancer and cataract, respectively, patients without behavior codes were excluded. Data for 15,407 breast cancer patients and 7,020 controls were analyzed before matching. After matching for comorbidities and age, either group comprised 2,252 patients. The median follow-up time was 104.1±24.0 months after matching. After matching, breast cancer was a predictor of a lower risk of for dementia (hazard ratio, 0.091; 95% confidence interval, 0.075 to 0.111; p < 0.001). In breast cancer patients, receiving chemotherapy and endocrine therapy did not significantly affect the incidence of dementia.
Conclusion
Breast cancer was associated with a remarkably decreased risk of dementia. The findings strongly suggest an inverse relationship between cancer and neurodegeneration, regardless of the adverse effects of cancer treatment on cognitive function.
Introduction
Breast cancer is the most common cancer among women. With the development of improved treatments and drug, the mortality rate of breast cancer has decreased annually by 2.3% [1,2]. The increased number of cancer survivors due to the improved survival outcomes has gradually increased the interest in their quality of life. Dementia, which is currently the most representative disease of the elderly, includes many subtypes, such as Alzheimer’s dementia, vascular dementia, dementia with Lewy bodies, frontotemporal dementia, and dementia in Parkinson disease [3,4]. The prevalence of all types of dementia increased gradually with increasing age [5,6], and this slowly debilitating disease remains irreversible and incurable.
Recent evidence has increasingly identified a significant inverse association between dementia and cancer [7,8]. In meta-analysis, patients with Alzheimer’s dementia had markedly lower co-occurrence of cancer in these individuals (pooled effect sizes, 0.32; 95% confidence interval [CI], 0.22 to 0.46) [7]. In addition, Yarchoan et al. [8], showed that participant with cancer history had significantly lower odds of Alzheimer’s dementia (odds ratio, 0.70; 95% CI, 0.55 to 0.89). In patients with dementia, the apoptosis tendency of cells can be expected to reduce the risk of cancer occurrence. Several biological pathway give credence to the theory that people who develop dementia may have some biological protective factors against cancer [9–12].
Nonetheless, there is limited strong evidence of an epidemiologic inverse association between breast cancer and dementia, possibly because of the relatively small study sample size [13], or sampling restricted to only some regions, indicating the lack of a nationwide population cohort [14]. Furthermore, previous studies did not focus on specific cancer types [15], making it very difficult to consider diversity between cancers or the effect of cancer treatment, including chemotherapy and endocrine therapy, which can negatively affect cognitive function (i.e., chemobrain) [16].
Therefore, we aimed to identify the risk of dementia in patients with breast cancer in a nationwide population-based cohort study. Furthermore, we evaluated the difference in the incidence of dementia according to the treatment modalities for breast cancer.
Materials and Methods
1. Study design and database
This retrospective observation cohort study used nationally representative data collected in the Korean National Health Insurance (NHI) claims database for a 12-year period from January 2009 to December 2018. In South Korea, it is mandatory for all residents to be affiliated to the national health insurance system, the NHI, which covers 97% of the population, except some foreigners who are ineligible for National Health Insurance. The database includes all medical claims provided by the Korean NHI Medical Services and the Korean Medical Aid program. The NHI database includes all medical data including: personal information, date of disease registry, diagnostic codes, procedure information, and prescription information. The disease codes specified in the International Classification of Disease, 10th revision (ICD-10), were used to record diagnoses in the NHI database. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies [17].
In this study, all individual information was anonymized prior to data processing to comply with the privacy guidelines of the Health Insurance Portability and Accountability Act in Korea. The study protocol was approved by the Institutional Review Board (IRB) of the Gangnam Severance Hospital (local IRB No. 3-2019-0425), which waived the need for informed consent based on the retrospective cohort design. This study was conducted in according with the ethical principles of the Declaration of Helsinki.
2. Study population
All female patients aged ≥ 50 years or older in the database were included in the initial screening stage. We included patients who had been diagnosed with breast cancer (ICD-10 code; C50) between 2009 and 2010, and who had not seen a physician for any type of cancer (ICD-10 code; C code) during the preceding 2-year period (2-year wash-out period prior to the study period). When extracting data among non-breast cancer patients from NHI database, massive data extraction was not permitted due to enormous data size. Inevitably, we chose senile cataract, a common benign disease, occurring in elderly patients. To select the generally healthy control group of subjects with conditions unrelated to the outcome of interest across the overall population, we extracted data of senile cataract (ICD-10 code; H25 and H26) under the same conditions as those for patients with breast cancer (2-year wash-out period between 2007 and 2008). In the breast cancer patients group, patients with a history of cataract were excluded from the analysis. The enrollment day for all subjects was the day of operation for breast cancer or cataract.
3. Predictor and outcome variables
The main outcomes of interest were the risk of all types of dementia (ICD-10 code; F00.0, F00.1, F00.2, F00.9, F01.0, F01.1, F01.2, F01.3, F01.8, F01.9, F02.0, F02.1, F02.2, F02.3, F02.8, F03, G30.0, G30.1, G30.8, G30.9, G31.0, G31.01, G31.02, G31.03, G31.04, G31.08, and G31.1) in patients with breast cancer. These codes include Alzheimer’s dementia, vascular dementia, dementia with Lewy bodies, frontotemporal dementia, dementia in Parkinson disease, and other types of dementia. The Korean government provides additional financial support to patients with breast cancer confirmed by pathologic evaluation. Therefore, the diagnostic code for breast cancer is highly reliable. To minimize misclassification errors, patients with breast cancer (ICD-10 code; C50) were defined as those who underwent breast cancer surgery between 2009 and 2010 (Behavior code; N7136, wide excision with axillary surgery; N7137, wide excision without axillary surgery; N7138, total mastectomy with axillary surgery; N7139, total mastectomy without axillary surgery). In the cataract group, to minimize the possibility of misclassification error, we defined cataract patients (ICD-10 code: H25 and H26) as those who underwent cataract surgery from 2009 to 2010 (Behavior code; S511, phacoemulsification and intraocular lens insertion). When entering the diagnosis code of dementia into a patient’s medical record, a clinician in Korea usually makes a diagnosis based on both his/her diagnostic impressions and test results such as Mini-Mental State Examination [18], Clinical Dementia Rating [19], and Global Deterioration Scale [20]. Magnetic resonance imaging scan or neuropsychological tests are also performed in many cases, however, there is a limit to the information provided from NHI, so that information could not be obtained. In this background, in view of the medical environment in Korea with the relative ease of visiting a physician, to increase the diagnostic validity of neurodegenerative disease, dementia was defined as at least 10 contacts with a physician to obtain a corresponding diagnostic code between 2011 and 2018.
A total of 90,396 subjects were identified in the breast cancer group and 85,906 subjects were selected from the cataract group. Each study participant was followed up until 2018 for the onset of dementia. Surviving participants without events until December 31, 2018 were censored after this time-point. The overall risks of any type of dementia were compared with those of the control group, and risks from receipt of endocrine treatment or chemotherapy in breast cancer patients were also evaluated.
4. Confounding variables
The confounding variable included several comorbidities and age. This study defined the confounding variables related to the development of dementia as follows: diabetes (ICD-10 code; E10, E11, E12, E13, and E14), hypertension (I10), hyperlipidemia (E78), chronic obstructive pulmonary disease (COPD; J44), chronic kidney disease (CKD; N18), liver cirrhosis (LC; K74 and K703), and heart failure (I50). Furthermore, we defined the presence of comorbidities as any diagnoses of the aforementioned codes in the 2 years preceding the enrollment date.
To reduce the selection bias, we estimated propensity scores for each of the all subjects to match the subjects who had breast cancer to those who had not. This was calculated for each subject with a logistic regression analysis, including variables of age and comorbidities. A nearest neighbor-matching algorithm with a “greedy” was performed to match the subjects using propensity score. We also used 1:1 propensity score matching to obtain the maximum number of patients with breast cancer and to minimize in the estimated results [21,22]. Randomization was performed using an algorithm within the SAS software program (ver. 9.4, SAS Institute Inc., Cary, NC). We explored the association of treatment modalities (chemotherapy, endocrine therapy, and use of aromatase inhibitor), comorbidities, and age with the incidence of dementia in the patients with breast cancer. In order to determine the effect of cataracts as a confounding factor for developing dementia, we also conduct sensitivity analysis the risk of dementia in the groups with concurrent cataract and breast versus with cataract only [23].
5. Statistical analysis
The primary endpoint was the overall risk of dementia in breast cancer patients compared to the age- and comorbidities-matched control group. The secondary endpoint was the difference in the incidence of dementia according to the treatment modalities for breast cancer. To compare the characteristics between the two groups, the Student’s t test was used for continuous variables, and the chi-square or Fisher exact test was used for categorical variables. The cumulative dementia incidences for two group were obtained using Kaplan-Meier curves and compared using the log-rank test. In a multivariable analysis, Cox proportional hazard models were used to determine the hazard ratio (HR) and 95% CI to investigate for the onset of dementia after adjustments for confounding variables. We applied the backward likelihood method (significance level for entering effect=0.05 and removing effects=0.05). A two-sided p-value less than 0.05 was considered to be statistically significant. Statistical analyses were performed using SAS software.
Results
1. Characteristics of the cohort population
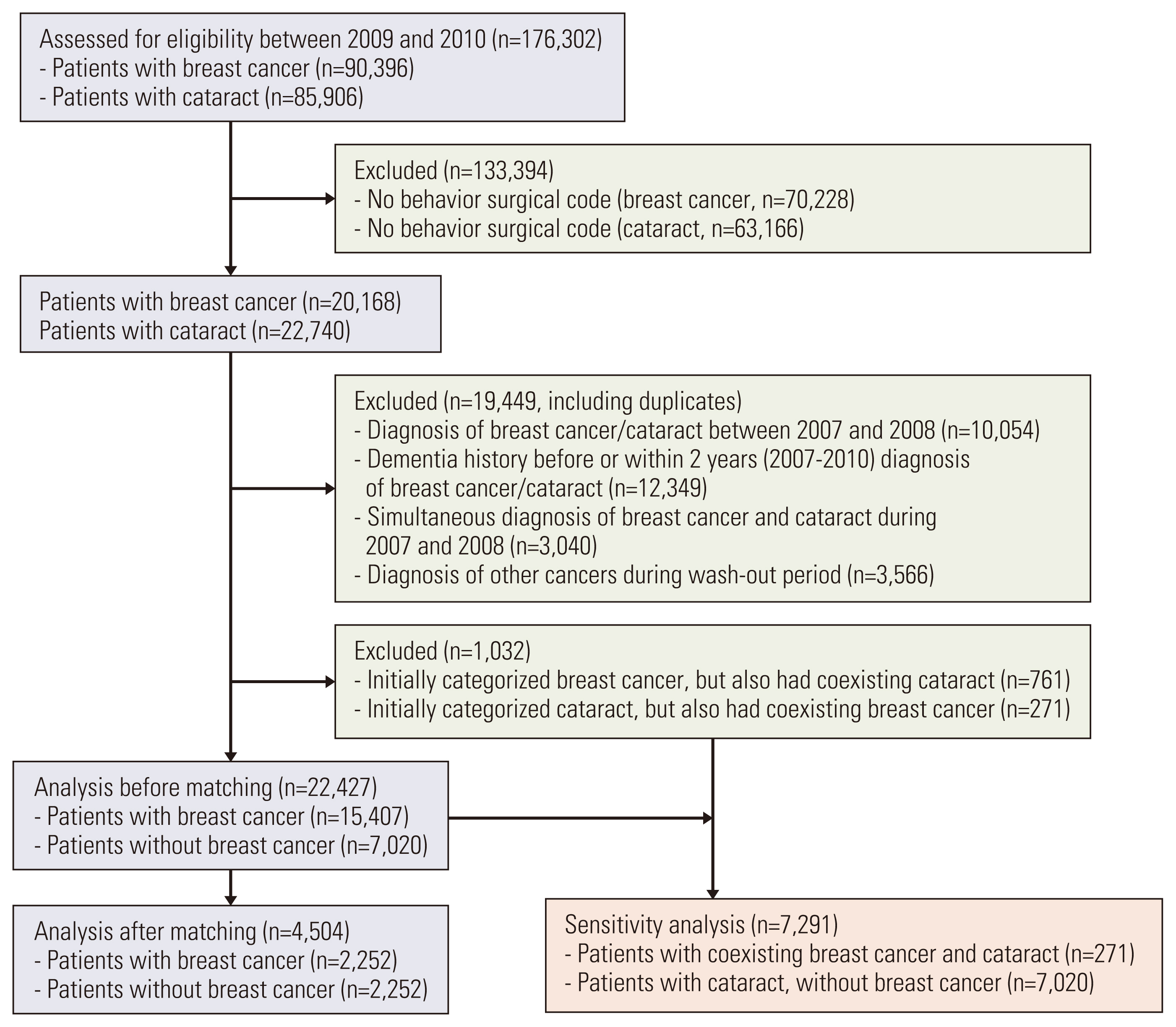
A total of 90,396 patients with breast cancer and 85,906 controls (patients with cataract) were assessed for inclusion in this study (Fig. 1). We excluded the patients without surgical behavior code (to select only new primary breast cancer patients), 20,168 patients with breast cancer, and 22,740 controls. After excluding patients who were diagnosed with cancer, cataract, and dementia prior to 2009 and those diagnosed with breast cancer and cataract simultaneously, there were 15,407 patients with breast cancer and 7,020 controls in the modified study sample. After matching, each group comprised 2,252 patients. Table 1 shows the between-group differences in the comorbidities and age of the patients. Before matching, the mean ages (±standard deviation), in patients with breast cancer and in controls were 53.73±7.59 and 73.39±7.78 years, respectively (Table 1). After matching, the mean ages in patients with breast cancer and in controls were 66.27±7.32 and 66.28±7.37 years, respectively (Table 1). Both groups were well-balanced with regard to comorbidities, such as diabetes, hypertension, hyperlipidemia, COPD, CKD, LC, heart failure, and age.
2. Risk analysis of dementia
Before matching, the median follow-up time was 104.1±24.0 months. Patients with breast cancer had a significantly low incidence of dementia (p < 0.001) (Fig. 2A). After matching, with a medial follow-up time of 103.3±25.4 months, patients with breast cancer had a statistically low incidence of dementia compared to controls (p < 0.001) (Fig. 2B). Of the 4,073 patients with dementia (166 and 3,907 dementia patients with and without breast cancer, before matching, respectively) (Table 1), dementia subtypes were classified as follows: 3,592 Alzheimer’s dementia, 185 vascular dementia, two frontotemporal dementia, nine dementia in Parkinson’s disease, 12 dementia with Lewy bodies, and 273 other types of dementia.

Kaplan-Meier analysis of incidence of dementia between patients with or without breast cancer. (A) Before matching, patients with breast cancer exhibited a low incidence of dementia than those without breast cancer (p < 0.001, log-rank test). (B) After matching, patients with breast cancer still had a low incidence of dementia (p < 0.001, log-rank test).
In univariable Cox proportional hazard analyses of the unmatched cohorts, diabetes, hypertension, hyperlipidemia, COPD, CKD, heart failure, age, and history of breast cancer were significantly associated inversely with incidence of dementia (Table 2). In the multivariable analysis of the unmatched cohorts, history of breast cancer (HR, 0.036; 95% CI, 0.030 to 0.043; p < 0.001) (Table 2) was a significant negative determinant of dementia after adjustment for comorbidities and age. In the cohort analyses of the Cox proportional hazard model after matching for comorbidities and age, the results showed that diabetes, hypertension, COPD, CKD, age, and history of breast cancer were significantly associated with a lower incidence of dementia (HR, 0.098; 95% CI, 0.081 to 0.119; p < 0.001) (Table 2). In the multivariable analysis, history of breast cancer was a significant lower predictor of dementia in the matched cohorts (HR, 0.091; 95% CI, 0.075 to 0.111; p < 0.001) (Table 2).
3. Subgroup analyses for incidence of dementia in breast cancer
The impact of treatment modalities on the incidence of dementia was evaluated in patients with breast cancer. Prior to matching, receiving chemotherapy (HR, 0.566; 95% CI, 0.417 to 0.767; p=0.002) (Fig. 3A); administration of endocrine therapy (HR, 1.981; 95% CI, 1.046 to 3.755; p=0.036) (Fig. 3A); the presence of diabetes, hypertension, hyperlipidemia, COPD, heart failure; and age were statistically significant factors for the occurrence of dementia among 15,407 breast cancer patients. The use of an aromatase inhibitor was not significantly associated with dementia (HR, 1.794; 95% CI, 0.665 to 4.839; p=0.248) (Fig. 3A). However, after adjustment for significant factors in the univariable analysis of unmatched cohort, receiving chemotherapy (HR, 1.371; 95% CI, 0.975 to 1.929; p=0.070; model 1: null model+chemotherapy) (Fig. 3B) and receiving endocrine therapy (HR, 1.386; 95% CI, 0.727 to 2.644; p=0.321; model 2: null model+endocrine therapy) (Fig. 3C) were not significantly associated with the risk for developing dementia. After matching, receiving chemotherapy (HR, 0.834; 95% CI, 0.575 to 1.209; p=0.337) (Fig. 3D) and endocrine therapy (HR, 1.549; 95% CI, 0.721 to 3.328; p=0.263) (Fig. 3D) did not significantly affect the incidence of dementia.
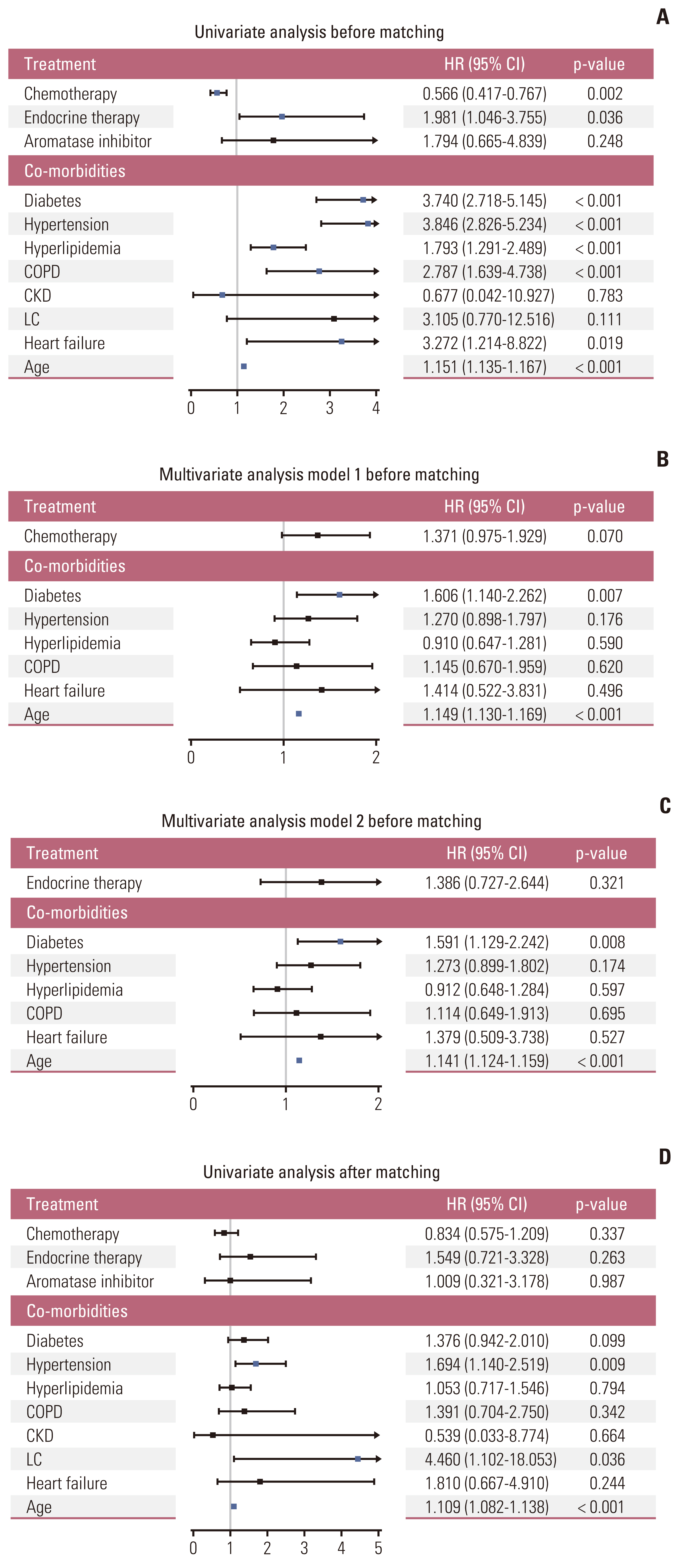
Subgroup analysis of incidence of dementia with stratification by treatment modalities, comorbidities, and age. (A) Before matching, receiving chemotherapy and endocrine therapy were related to the occurrence of dementia in univarate analysis (p=0.002 and p=0.036, respectively). (B) In multivariable model 1 (including receiving chemotherapy, but not endocrine therapy), the administration of chemotherapy was not a significant factor for dementia (p=0.070). (C) In multivariable model 2 (including receiving endocrine therapy, but not chemotherapy), receiving endocrine therapy was not a significant factor for dementia (p=0.321). (D) After matching, chemotherapy, endocrine therapy, and use of aromatase inhibitors did not significantly affected the incidence of dementia (p=0.337, p=0.263, and p=0.987, respectively). CI, confidence interval; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; HR, hazard ratio; LC, liver cirrhosis.
4. Sensitivity analysis for the incidence of dementia in breast cancer
To rule out whether cataracts affect the occurrence of dementia, a total of 7,291 patients (7,020 cataract patients without breast cancer and 272 patients with coexisting breast cancer and cataract) were included in sensitivity analysis (Fig. 1). Before matching, the median age was 73.26±7.80 and 67.78±9.01 years in the groups without and with breast cancer, respectively (p < 0.001) (S1 Table). In the univariable analysis, a history of breast cancer (HR, 0.113; 95% CI, 0.076 to 0.170; p < 0.001) (S2 Table), hypertension, hyperlipidemia, COPD, and age were significant factor for dementia. After adjustment, the history of breast cancer was a significant negative predictor of dementia in the multivariable analysis (HR, 0.138; 95% CI, 0.092 to 0.206; p < 0.001) (S2 Table). After matching, the two groups were well-balanced in terms of participant characteristics (S1 Table). In the univariable Cox proportional hazard model, breast cancer (HR, 0.176; 95% CI, 0.113 to 0.274; p < 0.001) (S2 Table), hyperlipidemia, and age were significant determinant of the risk for developing dementia. In the multivariable analysis of matched cohort, breast cancer was a significant predictor of a lower incidence of dementia (HR, 0.167; 95% CI, 0.107 to 0.259; p < 0.001) (S2 Table).
Discussion
The study investigated the risk of dementia in patients with breast cancer compared with that in control groups. To our knowledge, this is the first nationwide longitudinal cohort study that focused on breast cancer, after adjusting for comorbidities and considering the effect of cancer treatment, including chemotherapy, endocrine therapy, and treatment with aromatase inhibitors. On average, the breast cancer and control patients were followed over 8 years and, even after matching the cohorts for confounders, such as age and medical comorbidities, patients with breast cancer exhibited a remarkably lower risk of dementia. This finding is in line with previous findings [14] which showed an inverse correlation between cancer and neurodegenerative diseases, including dementia. This inverse relationship was robust; however, cancer treatment modalities, including chemotherapy and endocrine therapy, that can affect cognitive function [24] did not increase the risk of dementia. The findings of our study suggest the strong inverse relationship between dementia and breast cancer despite the negative impact on cognitive function during cancer treatment process. The understanding of the mechanism by which the onset of either cancer or dementia protects the development of the other may be of invaluable help in predicting cancer and dementia progression and developing novel treatments.
Considering the fact that we included cataract patients as a control group, that the visual symptoms of cataract and dementia overlap [25], and that cataract surgery may have an effect on cognitive function [25], within-group analysis (sensitivity analysis) was performed to confirm the findings of a lower risk of dementia in patients with breast cancer. Even within the group, the difference in the incidence of dementia according to the presence of breast cancer was clear. Therefore, breast cancer is considered to be a dependent factor for a lowing risk of the incidence of dementia.
With regard to the subtypes of dementia, more than 88% patients in this study were diagnosed with Alzheimer’s dementia. In contrast the diagnosis of breast cancer, which is considered definitive because it is a pathologic diagnosis, the diagnosis of the dementia subtype is only a clinical diagnosis. The data analyzed in this study were real-world nationwide data; thus, many physicians were not the specialists in cognitive disorders, such as doctor in primary care service. Therefore, some dementia subtype may have remained underdiagnosed. To overcome this limitation, we predominantly included only patients with multiple visits (at least 10 times) who experiencing cognitive decline and diagnosed with dementia by a doctor who clinically diagnosed the patients.
In the multivariable analysis after matching for age and comorbidities, old age was risk factors for dementia, however presence of breast cancer history was preventive factor for developing dementia. The results were similar to those of the within-group analysis of only cataract patients. Age is an important factor in determining the use of chemotherapy for breast cancer treatment. Fig. 3A indicates that chemotherapy is a protective factor in the occurrence of dementia in the univariable analysis before matching. Chemotherapy is primarily administered to relatively younger patients, and less often older patients, with breast cancer. Therefore, young age might have a protective effect on the low risk of dementia despite receiving chemotherapy. However, after matching, none of the treatment options influenced the incidence of dementia. An advantage of this study is that it focuses on only one cancer type, consider treatment options, and reveals that the effect of chemobrain is relatively insignificant compared to the protective effect of cancer itself.
This study had several limitations. First, as we mentioned, dementia was diagnosed by a clinician; therefore, the accuracy of the diagnosis of dementia cannot be guaranteed. Definitive diagnostic information, such as neuropsychological test or neuroimaging data, was unavailable in the insurance claims database. Second, because the NHI limits the amount of data that can be analyzed in one research project, and does not provide separate data for the matching control group, we inevitably collected data for cataract patients as a control group, not for healthy non-breast cancer subjects. Although there is no definite relationship between cataract and dementia in previous studies [26,27], there is a fundamental limitation in setting the control group in that cataract is a benign disease rather than non-breast cancer. However, this issue was partially addressed through a within-group sensitivity analysis. In addition, the NHI database is not digitalized before 2009, and it had the maximum observation period of eight to nine years. In this study, the diagnosis of dementia was defined as the number of visits by physician, it can lead to overestimation of dementia, including patients with minor cognitive impairment. Another limitation is that we observed outcome for almost 10 years, survived patients from breast cancer might be particularly resilient for diseases even though we only included patients who underwent curative resection. Lastly, although our sample size was large, we utilized longitudinal data, and the findings may not be generalizable to patients in other countries or patients of different ethnicities.
In this nationwide cohort study, breast cancer patients were inversely associated with the risk of developing dementia, regardless of cancer treatment options. This study provides further insight into the association between dementia and individual cancer types. This inverse relationship can serve as the basis for future research that can identify the biological mechanisms and novel treatment methods that can prevent neurodegeneration. Studies evaluating the association of dementia with other specific type of cancer are needed, considering the characteristics of the cancer type. Our findings require another large-scale external validation.
Electronic Supplementary Material
Supplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
Notes
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The protocol was approved by the Institutional Review Board (Local IRB No. 3-2019-0425) of Gangnam Severance Hospital. The need for informed consent was waived by the IRB due to the retrospective study design.
Author Contributions
Conceived and designed the analysis: Oh J, Seok JH, Yoon CI.
Collected the data: Oh J, Yoon CI.
Contributed data or analysis tools: Oh J, Lee HS, Jeon S, Yoo TK, Park WC, Yoon CI.
Performed the analysis: Oh J, Lee HS, Jeon S, Yoon CI.
Wrote the paper: Oh J, Lee HS, Yoon CI.
Conflicts of Interest
Conflict of interest relevant to this article was not reported.
Acknowledgments
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1C1C1007440). This work was also supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (Project Number: KMDF_PR_20200901_0186, 9991006856).