A Nationwide Survey of Knowledge of and Compliance with Cancer Pain Management Guidelines by Korean Physicians
Article information
Abstract
Purpose
Although cancer pain is prevalent, under-treatment still remains a problem. Knowledge of and compliance with guidelines for management of cancer pain were analyzed for exploration of physician-related barriers to cancer pain management. In addition, physicians' knowledge and its correlation with cancer pain control were audited.
Materials and Methods
From July 8 to December 2, 2010, a nationwide survey of house staff enquired about their knowledge of cancer pain control guidelines, and the medical records of patients under their care were analyzed.
Results
In total, 180 physicians participated in the study. Their average score for knowledge was 14.6 (range, 7 to 19; maximum possible, 20). When the knowledge score was divided into low, medium, and high scores, patients receiving care from physicians with high levels of knowledge tended to have better cancer pain control (p<0.001). Of the total patients with severe pain, 19.5% were not prescribed strong opioids, and 40% were not prescribed any medication for breakthrough pain.
Conclusion
Physicians' knowledge of guidelines for control of cancer pain showed an association with improvement of pain management. Overall adherence to the guidelines was lacking. Continuous interventions such as education and audits regarding cancer pain control guidelines for physician are needed.
Introduction
Chronic pain is the most frequent and troubling symptom in cancer patients. Prevalence rates from 33% during curative treatment to 64% in advanced/metastatic/terminal disease have been reported, with a pooled prevalence >50% for all cancer types [1]. However, the optimal pharmacotherapy is well established and sophisticated guidelines for control of cancer pain have become a standard tool in clinical practice, therefore, chronic cancer pain should be relieved in more than 90% of patients [2,3]. Although adequate and effective analgesic prescription is the key to control of cancer pain, a recent review reported that 43% of cancer patients had a negative pain management index score, meaning that prescription potency is inadequate when the patient's reported level of pain is compared with the intensity of the analgesic therapy [4]. The situation in Korea is similar. Despite increased attention to management of cancer pain, 47.4% of patients with severe pain did not receive adequate analgesia [5].
Why is there a difference between the ideal state and the real-world situation in cancer pain control? A recent review of the relevant literature identified several principal barriers to adequate management of cancer pain, including knowledge deficits, inadequate pain assessment, and misconceptions about pain on the part of both patients and professionals [6]. As expected, professional-related barriers included insufficient knowledge and poor evaluation of pain, lack of adherence to pain management guidelines, too much concern about addiction, and a low priority given to cancer pain control in treatment. Above all, several studies have reported that medical staff frequently have erroneous knowledge and simply do not pay attention to pain assessment [7,8,9,10]. Other factors such as reluctance to prescribe opioids, lack of access to opioids, and excessive regulation to prevent over-prescribing of opioids were demonstrated less frequently.
Thus, there is an urgent need for development of interventions that increase knowledge and adherence to existing cancer pain control guidelines for professionals. Studies on pain education programs for professionals have underscored the inadequacy of pain treatment; indeed, findings of three studies showed no difference in the decrease in patient pain between the intervention and control groups [11,12,13]. However, these studies targeted nurses. Because physicians are primarily responsible for prescribing medications, education of physicians in cancer pain control could have a greater impact. Kim et al. [14] reported on the effects of a pain education program for primary physicians who used the National Comprehensive Cancer Network (NCCN) guidelines for adult cancer pain. After receiving education, they classified physicians according to high and low guideline-observance groups and estimated the time to reach avisual analog scale pain score of <3. It took three days in the high guideline-observance group, but six days in the low observance group. These findings highlight the significance of continuous efforts to improve physician knowledge and audits of adherence to cancer pain management guidelines in the clinic.
In this study, we examined the knowledge of physicians who care primarily for cancer patients and their compliance with guidelines for management of cancer pain in clinical practice. In addition, we analyzed the correlation between a physician's level of pain management and the adequacy of pain control.
Materials and Methods
This study was approved by the institutional review board of each participating hospital. From July 8 to December 2, 2010, this study was conducted nationwide by means of a house staff survey and retrospective review of medical records.
The survey instrument was developed by the palliative care committee of the Korean Cancer Study Group. Four medical oncologists were actively involved in the process. Feedback and reviews were exchanged several times between investigators and protocol developers. Finally, 20 items were selected for evaluation of physicians' knowledge of pain management.
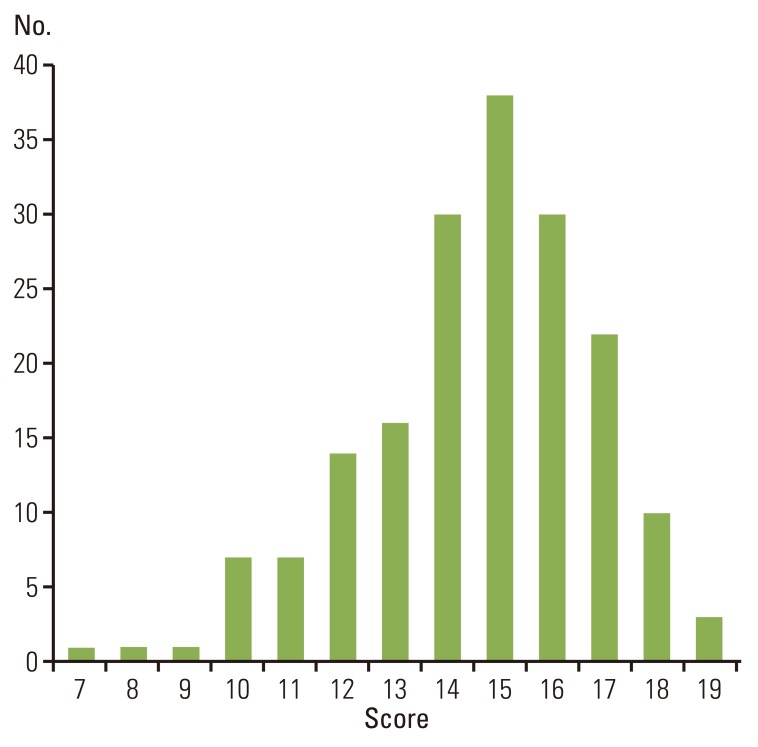
A survey of knowledge of NCCN adult cancer pain guidelines (ver. 1. 2011) was conducted among house staff responsible for the care of cancer patients. The questionnaire asked for information regarding the physician's age, gender, and practice setting. Of the 20 questions, 12 were answered with 'yes' or 'no,' while the other eight questions required selection of a single answer from among five multiple choice statements. The eight multiple-choice questions included three questions regarding treatment recommendations for hypothetical patients with challenging situations and five questions concerning specific pain management practices such as basic principles for the use of strong opioids and management of opioid side effects. Completion of the survey required 30 minutes, and it was intended to be answered before beginning the medical chart review.
The medical charts of patients under the care of physicians who completed the survey were reviewed retrospectively with respect to pain management three days prior to the date of the physician survey. The inclusion criteria were hospitalized patients who had ever complained of cancer pain, were receiving treatment from house staff who had completed the physician survey, had been hospitalized for more than four days, were over 20 years of age, and provided written informed consent.
Information regarding pain and pain management was obtained from medical records. The one-page data sheet covered five issues: 1) patient demographic data, including age, gender, diagnosis, stage, and Eastern Cooperative Oncology Group performance status scale; 2) pain assessment: severity, nature, and site; 3) management of chronic pain: drug composition and dose; 4) management of breakthrough pain: drug composition and dose; and 5) administration of drugs to counter the adverse effects of opioids.
Demographic characteristics of patients are presented as mean (standard deviation) or numbers and percentages. Physicians' knowledge of clinical practice guidelines was evaluated using 12 true/false questions; responses are presented as numbers and percentages. Physicians' responses regarding treatment strategies for challenging clinical scenarios are summarized as percentages. The linear association between pain severity classified using the numeric rating scale (NRS) on days -3 and 0 was evaluated using the Cochran-Mantel-Haenszel test. The chi-squared test was used to determine whether the change in the NRS level from day -3 to day 0 and the patient pain severity at day 0, grouped as none, mild, moderate, or severe, differed according to physician's level of knowledge. The grouping of NRS levels was based on the categorical pain scale of the NCCN guidelines: none (0), mild (1-3), moderate (4-6), or severe (7-10).
All statistical analyses were performed using SAS ver. 9.12 (SAS Institute Inc., Cary, NC). All p-values are two-tailed, and values of <0.05 were considered to indicate statistical significance.
Results
1. Subjects' characteristics
Among the 180 physicians who completed the survey, 95 (53.4%) were male. Their mean age was 29.6 years; 52.8% practiced in oncology wards, while the others practiced in hospice wards or other departments. The pain management audit was performed in 1,808 patients. Patient characteristics are shown in Table 1.
2. Evaluation of knowledge regarding clinical practice guidelines
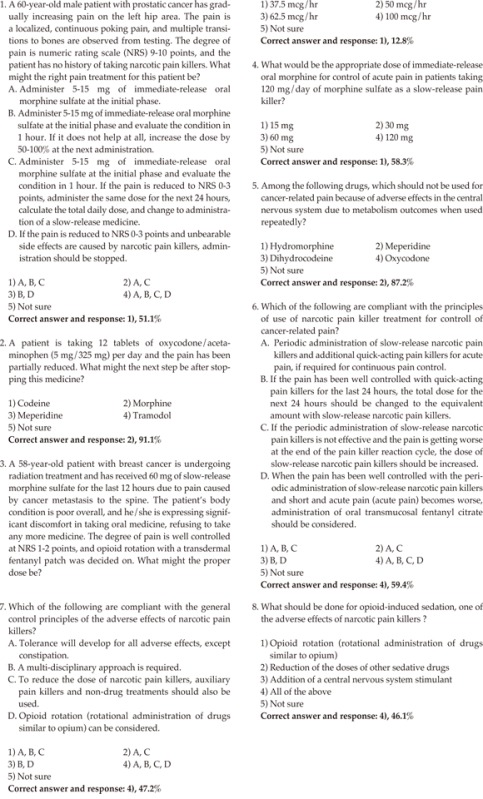
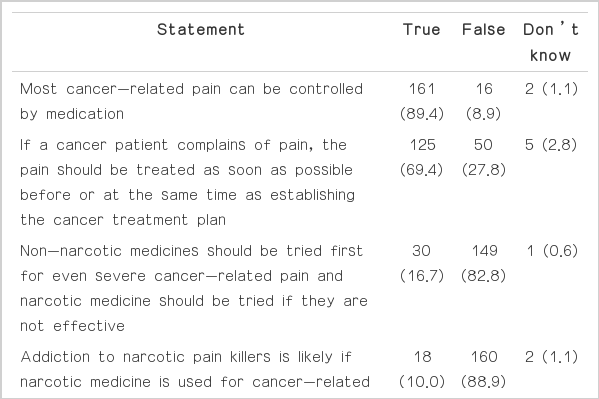
The distribution of knowledge scores is shown in Fig. 1. The average score for knowledge was 14.6 out of a maximum of 20 (range, 7 to 19). The 12 true/false questions and responses are listed in Table 2. Responses for the three hypothetical case scenarios and the remaining five questions, which required selection of one correct response from among multiple statements, are shown in Appendix 1.
The physicians answered the 12 true/false questions correctly 69.4% to 98.3% of the time. These questions concerned basic knowledge regarding cancer pain management. The questions most frequently answered incorrectly were those regarding a clinical scenario with equianalgesic dosing for opioid rotation (correct answer percentage, 12.8%), general principles of the adverse effects of opioids (correct answer percentage, 47.2%), and management of pain in opioid-naïve patients (correct answer percentage, 51.1%).
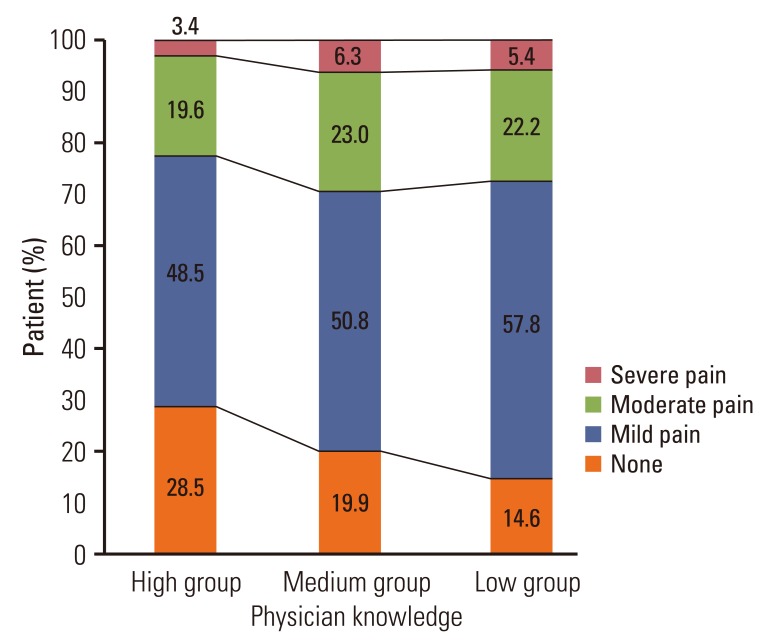
For interpretation of pain severity depending on a physician's knowledge level, physicians were divided into high, medium, and low subgroups. Cut-off values were set at 13 and 16 of the total of 20 points. The division by knowledge level-low, medium, and high-was 26.1% (47/180), 37.8% (68/180), and 36.1% (65/180), respectively.
3. Adherence in clinical practice to cancer pain management guidelines
Assessments performed included an audit of pain assessment records, medical records of pain assessment, and medications used for control of continuous and/or breakthrough pain.
The audit of pain assessment records showed that pain severity was recorded in 30.1% of cases, whereas other elements such as site of pain, nature of pain, and side effects of opioids were rarely recorded by the physician, in less than 5% of cases. Contrary to the World Health Organization (WHO) step-ladder analgesic guidelines, strong opioids were not prescribed to 19.5% of patients who complained of severe cancer pain. Pro re nata (PRN) prescriptions for control of breakthrough pain were not given to 40% of patients. Because the data were collected over four days, the parameters listed above were assessed on day 0; nevertheless, the results in terms of not prescribing strong opioids or PRN medications were similar on all days.
4. Pain severity and impact of physician knowledge
Based on the retrospective observations, the percentage of poorly controlled pain (NRS level higher than 4) during the three days before the survey was 33.2%. The average time for reduction of moderate and severe pain to mild pain was 1.74±0.8 days. Data on the change in pain severity from three days before the chart review day to the start day and its correlation with physician knowledge are shown in Table 3 and Fig. 2. Of those who complained of severe pain on day -3, 24.1% remained in severe pain on day 0. Patients under the care of physicians in the high-knowledge group tended to show a greater decrease in NRS level over time (p<0.001). A significant correlation was observed between pain severity on day 0 and physician's level of knowledge (Fig. 3) such that patients under the care of physicians with a high level of knowledge of cancer pain control tended to experience better cancer pain control. This finding was consistent during the four days of the medical chart review. Because pain severity was recorded by physicians only 30.1% of the time, nursing charts were also consulted. When both records were available for one patient, we found no significant difference in the NRS score between the physician record and the nursing chart. Thus, when both a physician record and a nursing chart were available for the same time period, we chose the physician record.

Correlation between changes of numeric rating scale (NRS) level and level of physician knowledge (p<0.0001).
Discussion
The current nationwide study demonstrated that many physicians lack knowledge of and compliance with cancer pain guidelines. In addition, the changes in and distribution of NRS levels were affected by the physicians' knowledge, suggesting that greater physician knowledge would translate to better patient outcomes.
Control of cancer pain has shown gradual improvement owing to more effective medications, better practice guidelines, and greater attention to pain management. Nevertheless, because pain management is inadequate in real-world situations, there remains significant room for further improvement [1].
Physician, patient, and regulatory issues are all well-known barriers to adequate pain management [6]. Physicians are primarily responsible for prescribing opioids and play a role in educating patients. Thus, apart from regulatory issues, overcoming physician barriers would seem to be an effective way of achieving cancer pain control. Many studies have supported the notion that professionals may possess inadequate knowledge and have concluded that a physician's inadequate assessment and knowledge of cancer pain contribute to poor pain management [15,16,17].
In the current study, we evaluated physicians' knowledge of cancer pain guidelines and its impact on severity of patients' pain. Although the overall score for knowledge was relatively high and almost 90% of physicians responded correctly to the true/false question on basic knowledge of cancer pain management, 27.8% answered no to a question regarding whether pain control was a priority. Indeed, most medical oncologists would readily perform active diagnostic imaging and/or anticancer treatment before pain control. However, many patients do not have to endure pain during evaluation and/or treatment. Pain control should be administered simultaneously with active evaluation/anticancer treatment. Increasing evidence in oncology of a link between survival and pain control supports the importance of this point [18]. Regarding questions with one correct answer among multiple choices, the three questions that were answered incorrectly most often concerned adequate pain control. Regarding equianalgesic dosing for opioid rotation, only 12.8% of responders answered correctly. The two other questions that were only infrequently answered correctly were queried general principles of the adverse effects of opioids (47.2%) and management of pain in opioid-naïve patients (51.1%). The correct answer for adequate breakthrough dosing was selected by only 58.3% of responders. These weak points were consistent with those of a study of knowledge of cancer pain management among physicians in British Columbia [19]. According to that study, equianalgesic dosing (68%) and adequate breakthrough dosing (45%) were the questions most commonly answered incorrectly.
Adherence to cancer pain guidelines by physicians on the wards is another key issue. Their competency in terms of knowledge, positive attitude, and skills under test conditions does not always translate into actual practice [20,21]. Major reasons for this may include time limitations on pain management due to busy rounds schedules and disparities between the tested and the actual circumstances.
A review of medical charts showed that strong opioids were not prescribed to 19.5% of patients with severe cancer pain, and 40% of total patients were not prescribed any medication for breakthrough pain. These data are surprising in comparison with the answers to the related survey questions. Indeed, 82.8% of responders answered "false" to the statement that non-narcotic medicines should be tried first even for severe cancer pain. In addition, 88.3% of physicians answered "yes" to the question of whether patients should have access to immediate-release opioids and be allowed to use them as needed for management of severe pain. Our findings are not unusual. Thota et al. [22] reported that only 48% of opioid prescriptions for chronic cancer pain were consistent with the WHO pain relief ladder, and only half of patients reporting severe pain were prescribed morphine.
Initially, we attempted to use the medication-assessment tool for cancer pain management (MAT-CP) for assessment of adherence to medication for control of cancer pain [23]. However, several criteria could not be analyzed consistently among patients. The representative parameters evaluated in this tudy were pain assessment as documented in the medical notes, WHO ladder drug combinations, and PRN prescriptions for intermittent pain. In a recent study using MAT-CT from the United Kingdom, overall adherence to guidelines was good, with low adherence (<50%) for nine criteria: documentation for pain intensity, characteristics, and etiology; pain intensity assessed before and after starting continuous opioids; normal-release preparation preferred; had morphine first; pain intensity recorded on follow-up pain therapy; and care issues for bone metastases, co-prescribing bisphosphonates [24]. Further work on the adequacy of opioid prescriptions, together with care issues such as side-effect management, is clearly needed in Korea.
Above all, our findings showed that better knowledge of cancer pain management resulted in greater reduction of patient pain severity. To date, use of five interventions for pain management in hospitalized cancer patients-professional and patient education, institution of regular assessments, audits of pain results and feedback to clinical staff, computerized decisional support systems, and specialist-level pain consultation services-has not led to improvement of severity of patient pain, although patient satisfaction was increased. However, the professional education was aimed primarily at nurses and did not specifically target physicians. Taking that into consideration, our finding is unique in suggesting that greater physician knowledge of cancer pain management would result in greater pain relief for patients.
This study has several limitations. First, the responding physicians may not be representative. In particular, knowledge and prescribing preferences were based primarily on medical oncologists. The findings might have been different had the survey included physicians of other specialties. Second, we were unable to determine correlation between physician knowledge levels and the extent of adherence to pain knowledge guidelines. As mentioned previously, we relied on clinical documentation obtained retrospectively from patient medical records. Thus, the information was not sufficient to evaluate correlation between a high level of knowledge and high adherence to guidelines.
Finally, further investigations regarding to determine whether physician knowledge is reflected in actual clinical practice and affects improvement of patient pain and patient satisfaction, and, ultimately, outcome should be conducted.
Conclusion
Our data suggest that systematic education and adherence to practice guidelines for management of cancer pain should be encouraged in all physicians responsible for care of patients suffering cancer pain. In addition, audits of adherence to cancer pain management guidelines should be conducted in order to ensure good pain management outcomes.
Acknowledgments
We would like to thank all institutions and physicians participating in this survey. Participating institutions are listed as follows.
Ajou University Medical Center, Asan Medical Center, Baptist Hospital, Bobath Memorial Hospital, Bohun Hospital (Daegu), Bohun Hospital (Gwangju), Bohun Hospital (Seoul), Bundang CHA Hospital, Bundang Jesaeng Hospital, Busan Medical Center, Busan St. Mary's Hospital, Cheongju St. Mary's Hospital, Chonbuk National University Hospital, Chonnam National University Hwansun Hospital, Chosun University Hospital, Chung-Ang University Hospital, Chungbuk National University Hospital, Chungnam National University Hospital, Daegu Fatima Hospital, Daegu Catholic University Medical Center, Dankook University Hospital, Dong-A University Hospital, Dongguk University Ilsan Hospital, Gyeongsang National University Hospital, Eulji University Hospital (Daejeon), Eulji University Hospital (Seoul) Medical Center, Ewha Womens University Mokdong Hospital, Gachon University Gil Hospital, Good Samaritan Hospital, Korea Cancer Center Hospital, Hanil Hospital, Hallym University Medical Center, Hanyang University Hospital, Inha University Hospital, Inje University Haeundae Paik Hospital, Inje University Sanggye Paik Hospital, Inje University Seoul Paik Hospital, Inje University Pusan Paik Hospital, Kangbuk Samsung Hospital, Keimyung University Dongsan Medical Center, Konkuk University Medical Center, Konyang University Hospital, Korea University Anam Hospital, Korea University Guro Hospital, Kosin Universiy Gospel Hospital, Kyung Hee University Hospital at Gangdong, Kyungpook National University Hospital, Medi-Yin Hospital, Myongji Hospital, National Health Insurance Service Ilsan Hospital, Pusan National University Hospital, Pusan National University Yangsan Hospital, SAM Anyang Hospital, Saemyung Hopsital, Samgsung Medical Center, Seoul Medical Center, Seoul Metropolitan Seobuk Hospital, Seoul National University Bundang Hospital, Severance Hospital, SMG-SNU Boramae Medical Center, Soonchunhyang University Hospital, Soonchunhyang University Bucheon Hospital, Soonchunhyang University Cheonan Hospital, St. Carollo Hospital, The Catholic University of Korea Bucheon St. Mary's Hospital, The Catholic University of Korea Daejeon St. Mary's Hospital, The Catholic University of Korea Incheon St. Mary's Hospital, The Catholic University of Korea Seoul St. Mary's Hospital, The Catholic University of Korea Yeouido St. Mary's Hospital, The Catholic University of Korea St. Paul's Hospital, The Catholic University of Korea Uijeongbu St. Mary's Hospital, Wonju Christian Hospital, Wonkwang University Hospital, Yeungnam University Hospital.
Notes
This research was supported financially by grants from the Johnson & Johnson family of companies, whose role was restricted and did not involve providing assistance to the investigators in the conception, conduct, and analysis of the study.
Appendices
Appendix 1