Case Series of Different Onset of Skin Metastasis According to the Breast Cancer Subtypes
Article information
Abstract
We report on five cases of skin metastasis according to the breast cancer (BC) subtype. Two cases of HER2 positive BC showed only skin metastasis after immediate postoperative period and rapid clinical response to targeted therapy. Another two cases of triple negative BC showed thyroid and lung metastasis in addition to skin metastasis, and their response of cytotoxic chemotherapy was not definite. The other hormone positive BC showed skin metastasis only, with a longer, slower, less progressive pattern than other subtypes. Most cases of skin metastasis were detected at terminal stage of malignancy and were considered to have a limited survival period. However, some BC patients can survive longer if the targeted agents are effective. Therefore, physicians should provide detailed follow up of BC after curative treatment and understand the metastatic pattern of BC according to the subtype.
Introduction
Breast cancer is a heterogeneous disease. Histologically similar tumors may have different prognoses and show different responses to therapy. These characteristics in clinical behavior are believed to be due to molecular differences [1]. Comprehensive gene expression profiling using DNA microarrays has identified five major molecular subtypes: luminal A, luminal B, human epidermal growth factor receptor2 (HER2), basal-like, and normal breast-like [2,3,4]. Basallike (mostly HER2 not amplified, and estrogen receptor [ER] and progesterone receptor [PR] negative) subtypes have the shortest relapse-free and overall survival rates, whereas luminal-type (ER and/or PR positive) tumors have relatively favorable clinical outcomes [3,5,6].
Skin metastasis of solid tumors accounts for 2% of all skin tumors. However, the rate of skin metastasis in patients with breast cancer is as high as 23.9% [7]. According to the pathogenesis of skin metastasis, tumor cells reach the skin through several routes: direct invasion from underlying structures, extension through lymphatics, embolization through lymphatics and blood vessels, and accidental implantation during surgery [8]. The anterior chest wall is the most common site of metastasis, however, other sites include the contralateral breast, scar sites, arms, and the head and neck region. Skin metastasis can present clinically in various patterns. For example, it can present as new skin nodules, the most common presentation, or ulcers, which are relatively less common. Other rarer clinical manifestations include erythematous patches or plaques. The clinical appearance of skin metastasis may even mimic benign dermatologic lesions, such as erythema annulare, contact dermatitis, tinea infections, erysipelas, cellulitis, and cutaneous mucinosis [9].
In general, skin metastasis is believed to be a manifestation of systemic metastasis, carry a limited survival period, and thus present as a terminal stage of malignancy. However, in the absence of internal visceral organ metastasis, some breast cancer patients with metastasis of skin only may have a good prognosis and prolonged survival. Some of them may even be cured of disease [10] using targeted agents, such as trastuzumab, used in treatment of the HER2 positive subtype.
In this study, we compare the onset time of skin metastasis, the clinical course and prognosis of these cases according to the breast cancer subtype, including two cases of HER2 positive breast cancer, two cases of triple negative breast cancer, and one case of hormone receptor positive breast cancer.
Case Reports
1. HER2 positive breast cancer
1) Case 1
A 40-year-old woman was diagnosed with cancer of the left breast (cT2NxM0) in June 2010. She received neoadjuvant chemotherapy with four cycles of doxorubicin and cyclophosphamide (AC), followed by four cycles of docetaxel. Afterwards, the patient underwent a total mastectomy and left axillary lymph node dissection (pT3N1M0) in October 2010. The pathology report showed ER and PR negative, but HER2 3+ positive by immunohistochemistry (IHC) and no skin and chest wall involvement with dermal lymphatic invasion. She subsequently started adjuvant radiotherapy and trastuzumab therapy (Fig. 1A).

(A) Before adjuvant radiotherapy after the operation. (B) Localized erythematous to purplish patch with multiple mass lesions measuring 1-2 cm in size on the left anterior chest four months after trastuzumab therapy, which was confirmed as a metastatic breast cancer. (C) The lesions showed rapid improvement after one cycle of clinical trial for pan-HER inhibitor.
After four months of adjuvant trastuzumab therapy, we found localized erythematous to purplish patch lesions, with multiple masses measuring 1-2 cm in size on the left anterior chest (Fig. 1B). A punch biopsy of the lesions confirmed metastatic breast cancer.
She enrolled in a clinical trial for pan-HER inhibitor of trastuzumab and failed due to recurrent breast cancer. She received chemotherapy with afatinib, pan-HER inhibitor plus vinorelbine in February 2012. After one cycle of treatment, her skin lesion showed rapid improvement (Fig. 1C). However, the same skin lesion showed progression again after six cycles of treatment. We applied lapatinib, another HER2 targeted, tyrosine kinase inhibitor, plus capecitabine after disease progression. After onlyone cycle of lapatinib treatment, the skin lesion showed improvement again.
2) Case 2
A 57-year-old woman was diagnosed with cancer of the left breast (cT4bN2M0) in January 2010. She received neoadjuvant chemotherapy with four cycles of AC. After that, we found that the primary breast mass size had increased and confirmed disease progression by imaging study. She underwent a left modified radical mastectomy (MRM) in April 2010 (T4N2M0). The pathology indicated ER and PR negative, but HER2 3+ positive by IHC and underlying fascia and muscle involvement and dermal lymphatic invasion. She thus started four cycles of adjuvant paclitaxel with trastuzumabin May 2010, followed by adjuvant trastuzumabtherapy until February 2011.
Ten days after the final trastuzumab treatment, she presented with an erythematous, annular, patch-like skin lesion with a central clearing on the left breast and lateral chest wall (Fig. 2A). The result of punch biopsy indicated a metastatic carcinoma in the dermal lymphovascular space of the breast. She received palliative chemotherapy with six cycles of capecitabine combined with lapatinib. After one cycle of capecitabine and lapatinib, the skin lesion showed rapid improvement (Fig. 2B). A complete response was maintained until nine cycles of this regimen. However, the same area of skin lesions showed progression again after nine cycles of lapatinib treatment. We retried trastuzumab therapy with another cytotoxic chemoagent, vinorelbine, combined with radiotherapy. After three cycles of chemotherapy, the skin lesions showed improvement (Fig. 2C).

(A) Localized erythematous annular patch with a central clearance lesion on the left breast and lateral chest wall 10 days after trastuzumab therapy, which was confirmed as a metastatic breast cancer. (B) The lesions showed rapid improvement after one cycle of capecitabine combined with lapatinib. (C) Three months after completion of lapatinib treatment, the lesion progressed and chemotherapy based on trastuzumab and vinorelbine with radiotherapy was started. After three cycles of treatment, the lesions showed an improved state.
2. Triple negative breast cancer
1) Case 1
A 44-year-old woman was diagnosed with cancer of the left breast (cT2N+M0) in August 2011. She received neoadjuvant chemotherapy with four cycles of AC. During treatment, a lymph node in the left supraclavicular fossa became palpable and suspicious for metastatic breast cancer. She underwent a left MRM and left axillary lymph node dissection (pT2N3M0) in December 2011. The pathology indicated triple negative breast cancer by IHC with no skin and chest wall involvement but showed dermal lymphatic invasion. She subsequently received adjuvant chemotherapy with three cycles of docetaxel.
During the fourth cycle of adjuvant docetaxel therapy, she presented with a localized erythematous patch and multiple papules with yellowish crusts near the operation scar on the left chest wall (Fig. 3A). A skin punch biopsy confirmed a metastatic carcinoma of the breast. She received combination therapy of gemcitabine plus cisplatin from April 2012. After four cycles of chemotherapy, the skin lesions showed waxing and waning without definite response (Fig. 3B).
2) Case 2
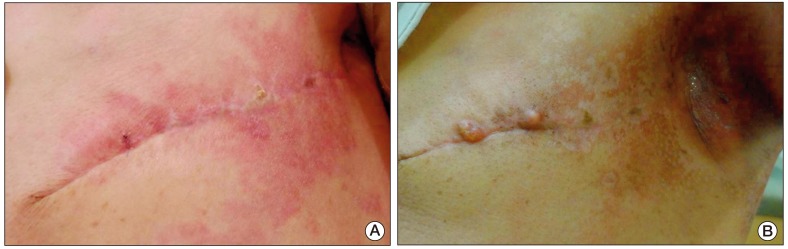
A 44-year-old woman was diagnosed with cancer of the left breast (cT3N+M0) in June 2011. She started neoadjuvant chemotherapy with four cycles of AC followed by docetaxelplus S-1 based on a clinical trial conducted in July 2011. After six cycles of neoadjuvant chemotherapy, the patient was admitted to the hospital due to an atypical pneumonia. Despite receiving treatment for atypical pneumonia, her condition did not show significant improvement. While receiving treatment for pneumonia, we found a skin lesion that was suspicious for a metastatic lesion. She underwent a left MRM for breast cancer, and a wedge resection of her lung via video assisted thoracoscopy for a suspicious lesion of cryptogenic organizing pneumonia in November 2011. The breast pathology indicated triple negative breast cancer by IHC with dermal lymphatic invasion, and the lung pathology showed metastatic breast cancer with the same histology. She started palliative chemotherapy with gemcitabine and cisplatin in February 2012. After three cycles of platinum based chemotherapy, we found that the skin lesions had progressed with localized, erythematous scaly plaques with brown pigmentation on the left chest wall (Fig. 4A). She received palliative radiotherapy for those lesions followed by cytotoxic chemotherapy with paclitaxel plus ifosfamide. The skin lesions subsequently stabilized (Fig. 4B). However, a newly developed liver lesion was found after four cycles of paclitaxel plus ifosfamide.

(A) Localized erythematous scaly plaque with brown pigmentations on the left anterior chest wall after adjuvant chemotherapy, which was confirmed as a metastatic breast cancer. (B) The lesion is on stable state after palliative radiotherapy and chemotherapy with paclitaxel and ifosfamide for three months.
3. Hormone positive breast cancer
A 62-year-old woman was diagnosed with cancer of the right breast with involvement of breast skin only (cT4bN+M1) 21 years ago. She had received neoadjuvant chemotherapy with four cycles of 5-fluorouracil, adriamycin, and cyclophosphamide followed by MRM. The pathology indicated no skin involvement, but tumor extension to underlying fascia, nipple, and areola. She received adjuvant treatment with radiotherapy and chemotherapy.
Nine years after initial treatment, skin lesions were found on her right arm, chest. A skin punch biopsy performed at another institute revealed a metastatic adenocarcinoma, which was ER and PR positive, and HER2 1+ by IHC. She had received chemotherapy and hormone therapy with all available drugs (tamoxifen, paclitaxel, letrozole, gemcitabine, capecitabine, anastrozole, docetaxel, exemestane, fulvestrant, 5-fluorouracil, vinorelbine) for refractory metastatic breast cancer.
Progression of metastatic skin lesions was detected in 2011. The lesion resembled a cluster of erythematous to yellowish verrucous masses (Fig. 5A). She visited our hospital and received salvage radiotherapy on her right upper extremity for one month. Even the skin lesions on her right arm showed improvement after radiation therapy (Fig. 5B). Progression of the skin lesions occurred once again (Fig. 5C). She was therefore treated with three cycles of cyclophosphamide, methotrexate, and fluorouracil. Without any response to cytotoxic chemotherapy her treatment was stopped due to poor general health.

(A) Multiple erythematous to yellowish verrucous masses on the right arm after 10 years of treatment. (B) The patient received a salvage radiotherapy for one month and the lesions showed improvement. (C) After three months, the lesion progressed and the patient received a palliative chemotherapy based on cyclophosphamide, methotrexate and 5-fluorouracil for three cycles, which was stopped due to poor general condition.
Discussion
Most skin metastasis of solid tumor presents at the terminal stage of advanced cancer, however, skin metastasis of breast cancer can arisein early phase of systemic metastasis according to the subtypes.
Skin metastases arising from hormone positive breast cancers can be treated with hormonal therapy, such as aromatase inhibitors. For this reason, evaluation of lesion biopsies with IHC can directly inform diagnosis and treatment [11]. Chemotherapy can be used when skin mestases are large or show rapid progression, or when metastasis does not respond to hormone therapy [12].
Most of the skin lesions appeared to be associated with a primary mass, and spread in a direct, contiguous nature, except for two skin lesions detected on the upper back and contralateral upper thorax, which were not related to any primary skin mass sites. This finding implies that skin metastasis in breast cancer may not only develop from primary breast cancers, but also from advanced disease. Thus, treatment should focus on control of systemic, rather than local disease [10]. For some cases involving a huge breast mass with ulceration, local radiation therapy is a useful tool for symptomatic control. Nevertheless, most skin lesions with or without soft tissue infiltration are not readily manageable by local modalities, such as surgery and/or radiation therapy, because skin and/or soft tissue infiltration are more likely manifestations of systemic relapse. Therefore, therapeutic strategies should be based on control of systemic disease rather than local modalities, even in patients with skin-only lesions [10].
In this case series, metastatic sites were limited mainly to the skin. In analysis of the subtypes of breast cancer, the first two HER2 positive subtype patients showed only skin metastasis. In the first case, skin lesions were observed approximately four months after completion of the curative treatment and skin metastasis presented approximately 10 days after treatment in the second case. In those two cases, the skin lesions showed rapid improvement after one cycle of anti-HER2 therapy. However, the lesions showed worsening immediately after a few cycles of anti-HER2 treatment. In the case of triple negative breast cancer subtypes, two cases of skin metastasis occurred during adjuvant or neoadjuvant chemotherapy. Unfortunately, despite receiving radiotherapy and systemic chemotherapy, their skin lesions did not show improvement, in contrast with HER2 positive subtype cases.
Skin metastasis appeared during or immediately after curative treatment in patients with the HER2 positive and triple negative breast cancer subtype. Another hormone positive subtype showed recurrence much later in the disease course. Skin lesions waxed and waned by repeated systemic chemotherapy and only showed temporary improvement after radiotherapy.
In conclusion, this case suggests that skin metastasis of some breast cancer subtypes probably arises earlier than from other solid malignancies. As seen in this case, HER2 positive breast cancer can show rapid improvement in response to targeted therapy or show progression due to early resistance, which can be the early sign of systemic metastasis and have poor prognosis if they do not response to the treatment. Therefore, physicians should perform a detailed physical examination for detection of skin metastasis, which should be treated with systemic chemotherapy in addition to targeted therapy and radiotherapy.
This study was conducted in order to determine the tendency of skin metastasis according to the breast cancer subtypes. This study has limitation due to its small sample size. Our results need to be validated through analysis of additional cases of skin metastasis according to the breast cancer subtypes in order to determine the clinical meaning.
Notes
Conflict of interest relevant to this article was not reported.