Isolated Diaphragmatic Metastasis Originated from Adenocarcinoma of the Colon
Article information
Abstract
Isolated diaphragmatic metastasis arising from colorectal cancer has been reported only one case in the literature presently. Here, we presented a new case and discussed the possible pathogenesis and the treatment options. A 42-year-old male patient had received anterior resection for sigmoid colon cancer. Although the increased serum CEA level was detected 20 months after the surgery, metastatic lesion could not be detected by repeated colonoscopy, CT scan, bone scan or PET scan for 35 months. We could detect a suspicious metastatic lesion on the liver by CT scan at 56 month after the surgery. During a second-look operation, we found a solitary metastasis on the diaphragm and removed it along with the 1 cm tumor-free resection margin. Although the prognosis associated with skeletal metastasis is poor, the complete resection of isolated diaphragmatic metastasis and subsequent appropriate adjuvant chemotherapy may achieve a cure the disease provided that other metastatic lesions are absent.
INTRODUCTION
The liver is the most frequent sites where distant metastasis occurs, followed by the lung, bone, and other sites (1). In a series of autopsies, the diaphragm was shown to be involved at the late stage of colon cancer, and usually as a part of disseminated disease (2). Recently, only one case of an isolated diaphragmatic metastasis in colon cancer has been reported. This metastatic lesion, however, showed a different cellular differentiation state from the primary lesion (3). Understanding of the mechanism of the development of diaphragmatic metastasis, early diagnostic modality, and appropriate treatment options will improve treatment outcomes.
CASE REPORT
A 42-year-old man presented with sigmoid colon cancer. The anterior resection along with the D2 lymph node dissection was performed. His preoperative serum CEA level was 77.4 ng/ml (<6 ng/ml). Distant metastasis was not detected by preoperative chest X-ray, CT (abdomen and pelvis) scan or during surgery. Histopathologic finding of the resected specimen showed moderately differentiated adenocarcinoma with abundant extracellular mucin confined to the colon wall. Metastasis was detected in two lymph nodes. His postoperative hospital stay was uneventful. His postoperative adjuvant therapy consisted of six cycles of intravenous 5-fluorouracil (375 mg/m2) and leukovorin (20 mg/m2). The patient was followed up every 3 to 6 months with complete blood count (CBC), liver function tests, serum CEA level and chest X-ray. CT scan of the abdomen and pelvis and colonoscopy were performed annually. His serum CEA level dropped gradually to 5.3 ng/ml 6 months after the surgery, and then fluctuated between 5.1 and 7.6 ng/ml for 20 months after the surgery (Fig. 1).

Clinical course of the patient: the close correlation between serum CEA level and treatment response.
Twenty months after the surgery, his serum CEA level gradually increased to 12.1 ng/ml. However, the recurred disease was not detected by colonoscopy or CT scan of the chest, abdomen, and pelvis or bone scan, suggesting that the increase of serum CEA was due to occult metastasis. The patient was treated with oral 5-FU [UFT®, tegafur (100 mg) & uracil (224 mg)/tablet, Jeil Pharm. Co., LTD., Seoul, Korea] 400 mg/day for 6 months, at which time his serum CEA level had returned to the normal range, but it rose again 4 months later. Repeated examination including colonoscopy, CT scan and bone scan did not reveal the recurrent disease. In addition, the evidence of recurrent disease was not detected on a positron emission tomography (PET) scan performed 51 months postoperatively. At 56 months postoperatively, however, we were able to detect a suspicious metastatic lesion at the 7th segment of the liver on CT scan. MRI showed a metastatic lesion at the same location (Fig. 2). The serum CEA level rose to 23.1 ng/ml by this time.
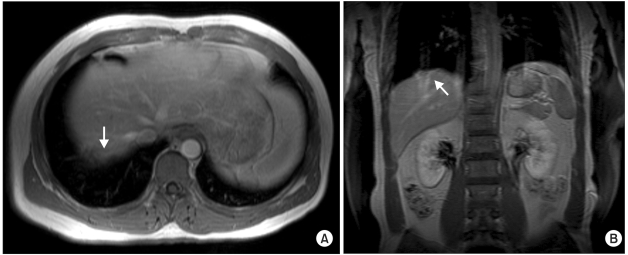
MRI of an isolated metastatic tumor on the diaphragm. (A) Gadolinium enhanced T1-weighted axial view showed a ill-defined peripherally enhanced low signal lesion (arrow). (B) coronal view showed a protruding mass with motion artifact (arrow).
Immediately after the confirmation of metastasis, the patient was returned to surgery. During the operation, we detected a solitary metastatic nodule on his diaphragm, facing the 7th segment of the liver. The lesion did not involve any other organs including the liver and the lung. We removed the tumor along the tumor-free resection margin at least 1 cm and repaired the defect. Histopathologic examination revealed a tumor measuring 2.6×0.7×0.5 cm that infiltrated the entire layer of the diaphragm. The tumor showed the same characteristic of the original sigmoid colon cancer, in regard to the state of differentiation and the amount of mucin (Fig. 3). Three weeks after the surgery, the patient's serum CEA level had returned to the normal range. Postoperative adjuvant therapy consisted of six cycles of intravenous irrinotecan (150 mg/m2), 5-FU (1,000 mg/m2) and leukovorin (20 mg/m2). Seventeen months after the surgery, the patient is alive with no evidence of disease.
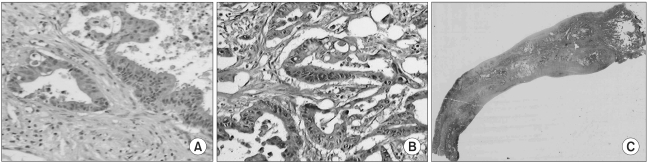
Histopathological findings. (A) primary sigmoid colon cancer (H&E, ×200). (B-C) isolated metastasis on the diaphragm. The metastatic tumor, which involved entire thickness of the diaphragm, had a moderate cellular differentiation and amount of mucin similar to that of the primary sigmoid colon cancer (H&E, ×200, ×40).
DISCUSSION
Distant metastasis of colorectal cancer occurs by lymphatic or hematogenous spread. In 50% of patients with colorectal cancer, circulating tumor cells were detected in the peripheral blood at the time of surgery (4). However, genuine hematogenous metastasis to the diaphragm is extremely rare. In our case, the route of metastasis may be either lymphatic or hematogenous. Since the majority of lymphatic metastasis occurs in a stepwise fashion and no apparent lymph node metastasis was detected during the second-look operation, we speculated that the likely route of metastasis in our patient is hematogenous.
The serum CEA level is a simple and sensitive marker for identifying recurrence or metastasis in colon cancer. In colon cancer patients, following complete surgical resection of colorectal carcinoma, the serum CEA level decreases to the normal range usually within one month in most cases, although it may take as long as 4 months (5). Thus, the serum CEA level of all colorectal cancer patients underwent curative resection should be measured. In patients whose serum CEA level fails to drop to the normal range, physicians should consider the possibility of the presence of hidden malignant foci or early recurrence (6).
Patients with the increased serum CEA level but no evidence of recurrence on imaging studies present a particular challenge to physicians. The options available are continued surveillance, a second-look operation, or the initiation of systemic chemotherapy. The options, however, have significant drawbacks. Continued surveillance may be frustrating for both clinicians and patients. Although the CEA-directed second-look operation detects the resectable recurred tumors in approximately 50% patients and achieves 5-year survival in one third of the patients, approximately 50% patients underwent the non-curative surgery (7,8). In regard to systemic chemotherapy, it is often difficult to justify because of its side effects and limited benefits. Thus, the improvement of the current diagnostic modalities and new diagnostic methods may lead to the early detection of recurrent colon cancer.
Since skeletal metastasis usually occurs as the consequence of systemic spread, the prognosis of patients with skeletal metastasis is poor. In one report, three out of four patients died of disease (9). The diaphragm is composed of voluntary muscles and relatively avascular fibrous tissues. The prognosis of diaphragmatic metastasis may be similar to skeletal metastasis. Nevertheless, the complete resection of the metastatic lesion and appropriate adjuvant systemic chemotherapy may achieve the cure in the absence of other metastatic lesions.