Pegfilgrastim Prophylaxis Is Effective in the Prevention of Febrile Neutropenia and Reduces Mortality in Patients Aged ≥ 75 Years with Diffuse Large B-Cell Lymphoma Treated with R-CHOP: A Prospective Cohort Study
Article information
Abstract
Purpose
Febrile neutropenia (FN) can cause suboptimal treatment and treatment-related mortality (TRM) in diffuse large B-cell lymphoma (DLBCL) patients treated with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP).
Materials and Methods
We conducted a prospective cohort study to evaluate the effectiveness of pegfilgrastim prophylaxis in DLBCL patients receiving R-CHOP, and we compared them with the PROCESS cohort (n=485).
Results
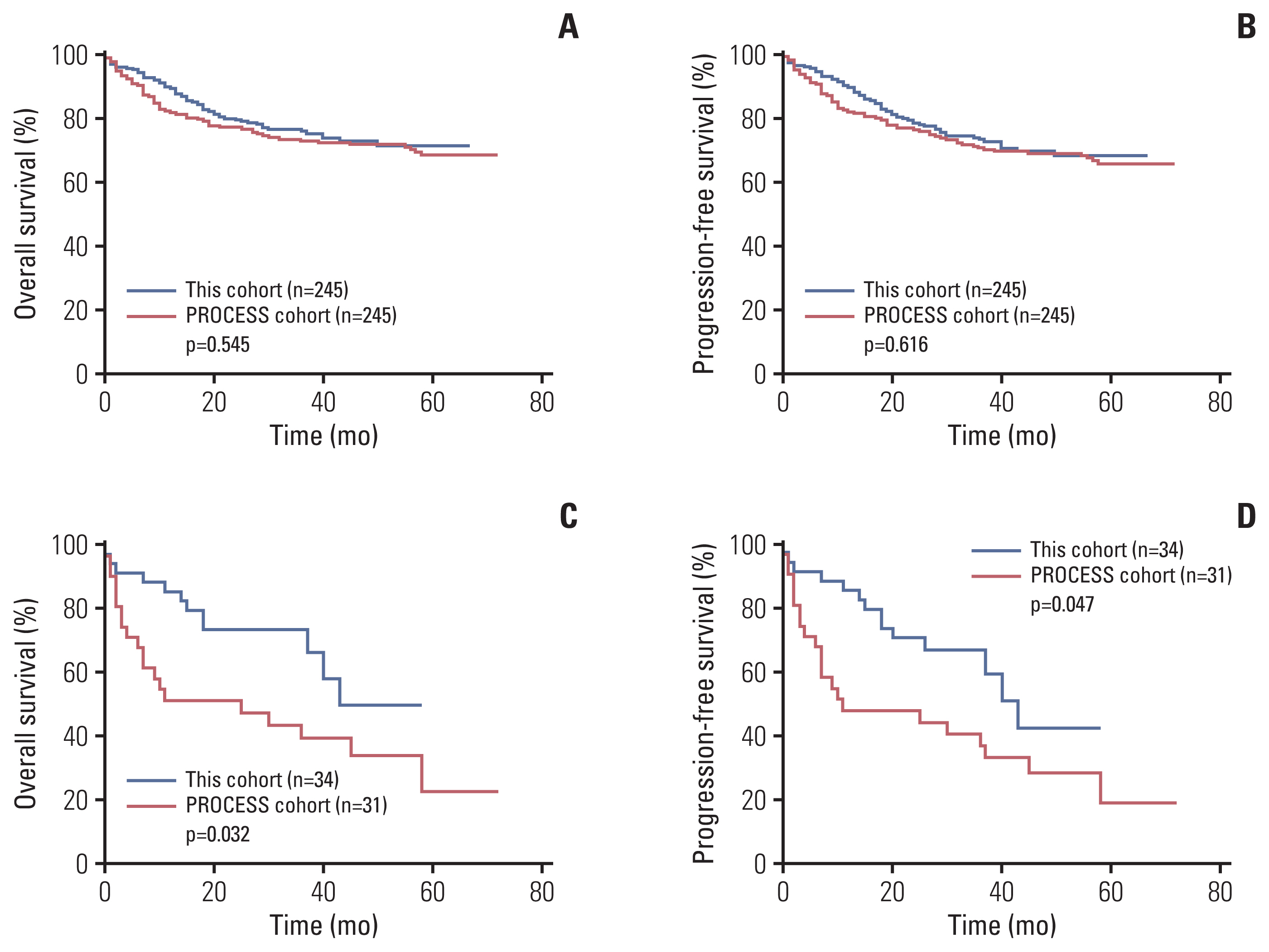
Since January 2015, 986 patients with DLBCL were enrolled. Pegfilgrastim was administered at least once in 930 patients (94.3%), covering 90.3% of all cycles. FN developed in 137 patients (13.9%) in this cohort (23.7% in the PROCESS cohort, p < 0.001), and 4.2% of all cycles (10.2% in the PROCESS cohort, p < 0.001). Dose delay was less common (≥ 3 days: 18.1% vs. 23.7%, p=0.015; ≥ 5 days: 12.0% vs. 18.3%, p=0.023) in this cohort than in the PROCESS cohort. The incidence of TRM (3.2% vs. 5.6%, p=0.047) and infection-related death (1.8% vs. 4.5%, p=0.004) was lower in this cohort than in the PROCESS cohort. The 4-year overall survival (OS) and progression-free survival (PFS) rates of the two cohorts were not different (OS: 73.0% vs. 71.9%, p=0.545; PFS: 69.5% vs. 68.8%, p=0.616). However, in patients aged ≥ 75 years, the 4-year OS and PFS rates were higher in this cohort than in the PROCESS cohort (OS: 49.6% vs. 33.7%, p=0.032; PFS: 44.2% vs. 30.3% p=0.047).
Conclusion
Pegfilgrastim prophylaxis is effective in the prevention of FN and infection-related death in DLBCL patients receiving R-CHOP, and it also improves OS in patients aged ≥ 75 years.
Introduction
Rituximab, cyclophosphamide, doxorubicin, and prednisolone (R-CHOP) is the standard treatment for patients with diffuse large B-cell lymphoma (DLBCL) and cures 60%–70% of patients [1,2]. Since the advent of chemoimmunotherapy, there has been no major breakthrough in terms of the frontline treatment for DLBCL. Therefore, supportive measures to reduce preventable treatment-related mortality (TRM) are very important for optimal treatment outcomes. One of the most important side effects of R-CHOP is febrile neutropenia (FN) caused by bone marrow suppression. TRM as well as suboptimal treatment may occur because of treatment delay, unplanned dose reduction, and discontinuation of chemotherapy due to FN [3]. In addition, FN causes additional medical costs in terms of need for hospitalization and antibiotic therapy [4,5]. Therefore, proper prevention and treatment of FN are crucial for achieving the best treatment outcomes with R-CHOP.
The reported incidence of FN with R-CHOP therapy varies (18%–23.8%) in many studies [1,3,6,7]. It was higher in patients who had risk factors such as older age, poor performance status, advanced disease, comorbidities, low serum albumin level, low baseline blood cell counts, low body surface area/body mass index, and absence of granulocyte colony-stimulating factor (G-CSF) prophylaxis [8–11]. As per clinical guidelines, primary prophylaxis with G-CSF or pegfilgrastim is recommended for patients planning to undergo chemotherapy if the assessed risk of FN is higher than 20% [6,12]. However, in real-world practice, primary prophylaxis is underutilized notwithstanding clinical guidelines [13]. For primary prophylaxis, use of pegfilgrastim is desirable as it needs to be administered only once per cycle because of its neutrophil-mediated pharmacokinetics, whereas other G-CSFs needs to be administered on a daily basis [14–16]. In addition, pegfilgrastim prophylaxis was associated with a reduced risk of neutropenia-related or all-cause hospitalization relative to filgrastim prophylaxis in a large-scale retrospective analysis [17]. Mean per-cycle neutropenia-related costs were also lower with pegfilgrastim than with filgrastim [16].
As pegfilgrastim prophylaxis became available for cancer patients in Korea in 2014, and the reported incidence of FN was higher than 20% among Korean DLBCL patients treated with R-CHOP [7], we prospectively collected data on primary prophylaxis with pegfilgrastim (GIRAFFE-B cohort) and compared them with the data obtained from a previous cohort enrolled in the same setting (PROCESS cohort) [18,19] to evaluate the benefits of pegfilgrastim prophylaxis in DLBCL patients treated with R-CHOP (ClinicalTrials.gov Identifier: NCT02474550).
Materials and Methods
1. Patients
The current cohort included patients with newly diagnosed DLBCL of any subtype according to the World Health Organization 2008 classification, who were planning to receive standard R-CHOP 21 as the primary treatment, planning to receive pegfilgrastim prophylaxis, aged 18 or older, and who had provided written informed consent. Patients with primary central nervous system (CNS) lymphoma or other concomitant malignancies that needed treatment or who had previous chemotherapy or radiotherapy were excluded. The study was conducted at 24 hospitals belonging to the Consortium for Improving Survival of Lymphoma (CISL) in Korea. The protocol was reviewed and approved by the institutional review board of each participating center, and all patients provided written informed consent before treatment initiation. The PROCESS cohort recruited patients from 27 hospitals belonging to the CISL between August 2010 and August 2012 to investigate CNS involvement in DLBCL. It also recruited newly diagnosed DLBCL patients with similar inclusion criteria as those used for the current cohort, except that it included patients aged ≥ 20 years and R-CHOP was administered without G-CSF prophylaxis [18].
2. Treatments
Patients were treated with the standard R-CHOP 21 regimen [1]. After enrollment, patients received up to 6–8 cycles of R-CHOP therapy. The number of cycles was reduced to 3–4 cycles in patients with stage I/II disease that was completely resected or who were about to undergo radiotherapy. CNS prophylaxis was performed at physician’s discretion. Patients received pegfilgrastim 6 mg (Neulasta, Amgen Manufacturing Ltd., Juncos, Puerto Rico) injection subcutaneously at least 24 hours after the completion of chemotherapy. Dose modification of the standard R-CHOP therapy and deferral of treatment were performed according to the physician’s decision. Concomitant use of prophylactic antibiotics was also allowed according to the institutional policies.
3. Study endpoints
The primary endpoint was the incidence of FN during and within 30 days of R-CHOP treatment.
FN was defined as a single oral temperature ≥ 38.3°C or ≥ 38.0°C for ≥ 1 hour with a neutrophil count of ≤ 0.5×109/L or a neutrophil count ≤ 1.0×109/L which was predicted to fall below 0.5×109/L. The secondary endpoints were as follows: (1) the delivery of planned treatments including dose delay of > 3 days and > 5 days, dose reduction of > 20%, relative dose intensity (RDI) of doxorubicin and cyclophosphamide, and average RDI (ARDI); (2) infection-related death and TRM within 6 months from the start of treatment; and (3) response to R-CHOP treatment, overall survival (OS) and progression-free survival (PFS). RDI for each agent was defined as the proportion of the standard dose intensity delivered. ARDI was calculated by averaging the delivered RDIs of cyclophosphamide and doxorubicin. OS was calculated from the time of diagnosis to the date of the last follow-up or death from any cause. PFS was calculated from the date of diagnosis to the date of relapse or progression, the last follow-up, or death from any cause. Response to therapy was evaluated according to the Lugano response criteria for non-Hodgkin lymphoma (NHL) [20]. Follow-up data including survival and disease status were updated and centrally reviewed every 6 months.
4. Statistical analysis
Statistical analysis was performed using SPSS ver. 25.0 software program for Windows (IBM Corp., Armonk, NY). We used a Fisher’s exact test to identify the associations between categorical variables. The time variable was estimated based on Kaplan-Meier curves and compared using a log-rank test. A Cox-regression hazard model was used for univariate and multivariate analyses. To define the risk factors for FN, a multivariate analysis was performed including variables with a p < 0.1 in a univariate analysis. A two-sided p < 0.05 was considered statistically significant. Propensity score matching (PSM) using parameters included in international prognostic index (IPI) and sex was performed to compare survival between the cohort of this study and the PROCESS cohort to minimize selection bias. In the present study, 1:1 nearest neighbor matching was performed using SPSS.
Results
1. Characteristics of patients
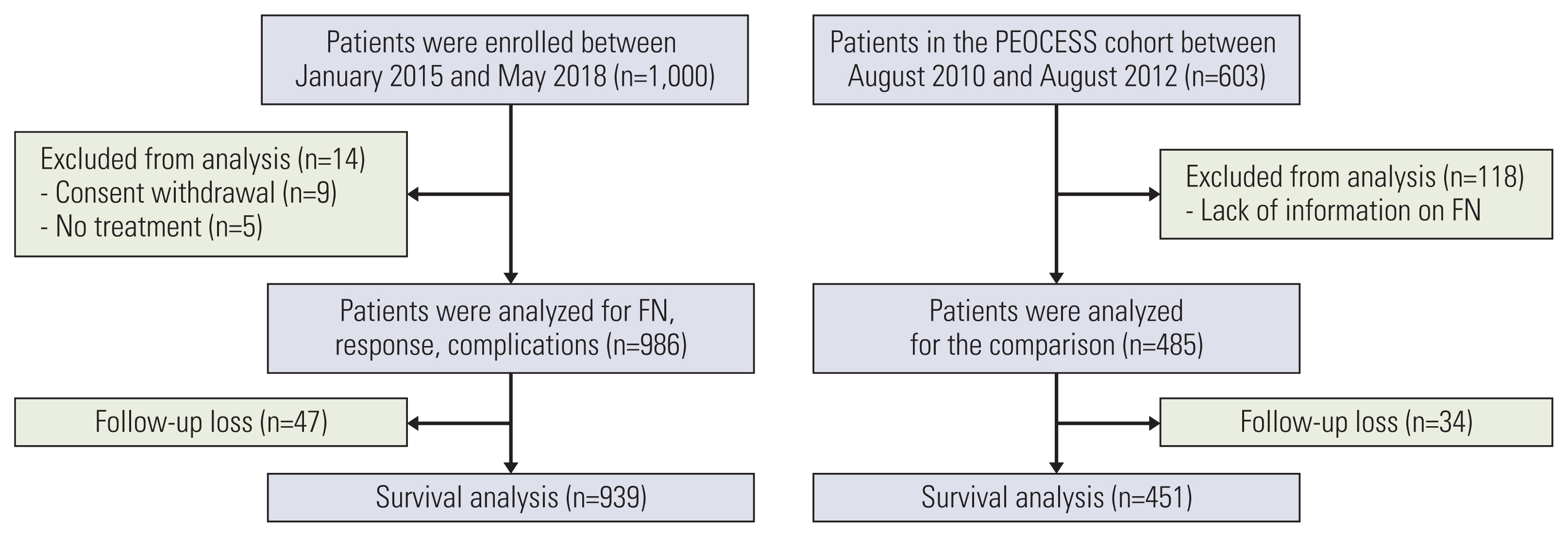
A total of 1,000 patients were enrolled in the GIRAFFE-B cohort from January 2015 to May 2018. Of these, nine patients withdrew consent, and five patients did not receive R-CHOP treatment. Thus, 986 patients who received at least one cycle of R-CHOP were included in the analysis. From the PROCESS cohort, 485 patients who had information available regarding the incidence of neutropenia and FN were included (Fig. 1). The overall characteristics of the analyzed patients did not deviate from those of all patients in the PROCESS cohort [18].
The characteristics of the patients in both cohorts are summarized in Table 1. The median age of the patients included in this study was 62 years (range, 19 to 86 years), which was 3 years higher than in the PROCESS cohort (range, 20 to 89 years). However, the proportion of patients aged ≥ 65 years and ≥ 75 years was not significantly different between the two cohorts.
2. FN and TRM with pegfilgrastim prophylaxis
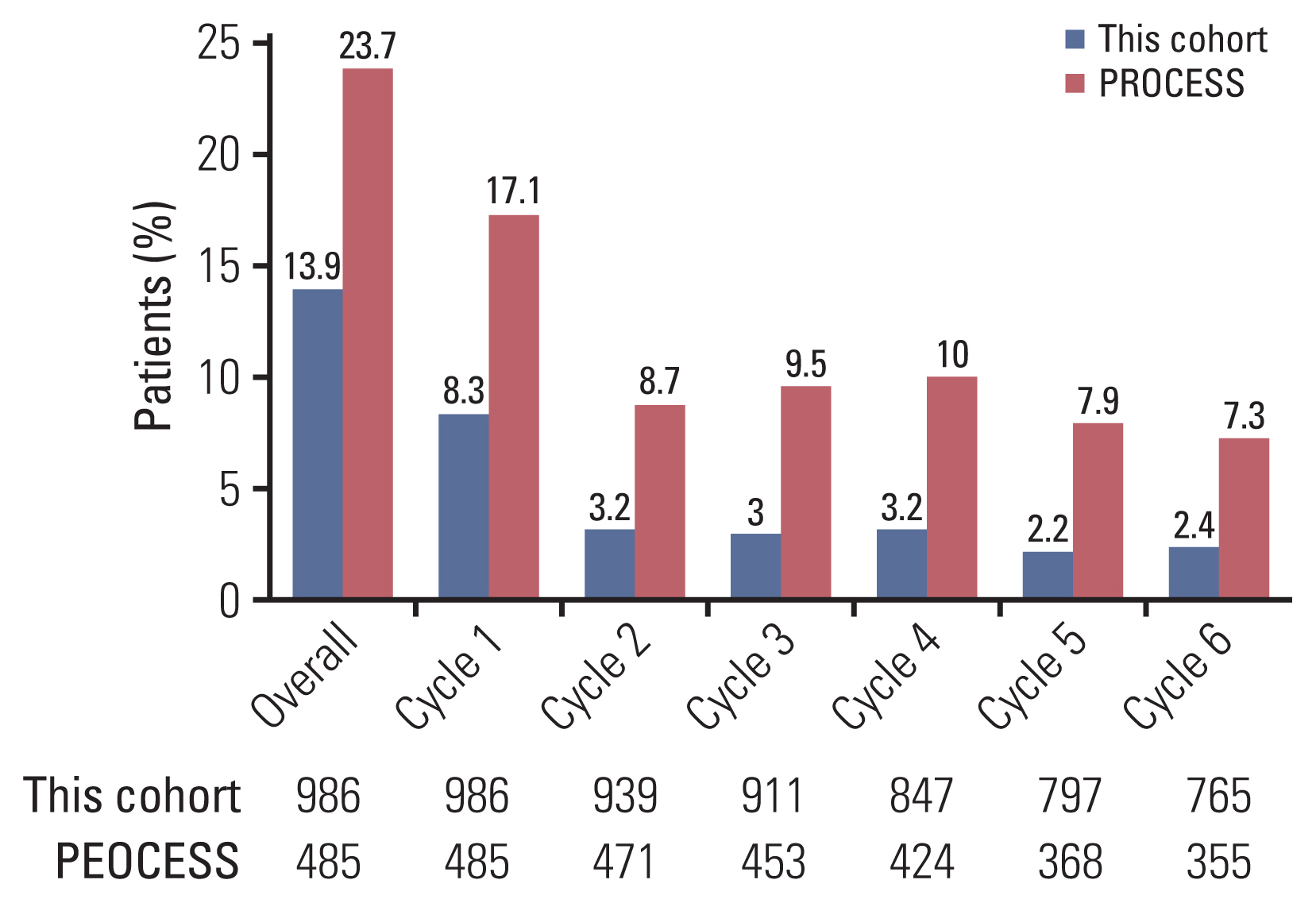
Pegfilgrastim prophylaxis was administered at least once to 930 patients (94.3%) in this cohort. The overall prophylaxis rate was 90.3% (4,831 doses in 5,348 cycles). The overall incidence of FN was 4.2% (222 events in 5,348 cycles) in this cohort (Table 2). Throughout the treatment course, 137 patients (13.9%) experienced at least one episode of FN in this cohort, whereas 23.7% (115/485) of the patients experienced FN in the PROCESS cohort, with an overall incidence of 10.2% (264 events in 2,581 cycles). Forty-five patients (32.8%) experienced multiple episodes of FN in this cohort. In the PROCESS cohort, 49 patients (42.6%) had multiple episodes, which included up to six events. Grade 4 neutropenia was reported in 286 patients (28.8%) and occurred in about 11.7% of the cycles in this cohort, which was significantly lower than that in the PROCESS cohort (Table 2). FN developed at a median of 7 days after treatment (range, 5 to 30 days). The incidence of FN was highest in the first cycle (8.3%) and decreased in the subsequent cycles. The risk reduction rate of FN with pegfilgrastim prophylaxis was higher in subsequent cycles than in the first cycle (Fig. 2).
In this cohort, TRM was significantly lower than that in the PROCESS cohort (3.2% vs. 5.6%, p=0.047), which was mainly due to lower incidence of infection-related death (1.8% vs. 4.5%, p=0.004) (Table 2). In particular, eight patients (11.6%) died of infection among patients aged ≥ 75 years in the PROCESS cohort, but only five deaths (3%) were infection-related in this cohort (p=0.023). TRM of non-infectious causes was not different between the two groups (1.4% vs. 1.0%, p=0.535), which includes intracranial hemorrhage, cardiac event, pneumothorax, acute exacerbation of chronic obstructive pulmonary disease, hepatic failure and bowel infarction.
3. R-CHOP treatment with pegfilgrastim prophylaxis
Overall, 765 patients (77.6%) completed six cycles of R-CHOP in this study, which was not significantly different from that in the PROCESS cohort (73.2%, p=0.069) (Table 3). In terms of dose delay, 179 patients (18.1%) experienced dose delay of > 3 days, and 119 patients (12%) had a dose delay of > 5 days (Table 3). In the PROCESS cohort, more patients experienced treatment delay (> 3 days in 23.7% and > 5 days in 16.5%) than that in this cohort. As for dose reduction of > 20%, this cohort showed a slightly higher doxorubicin reduction tendency compared to the PROCESS cohort (19.5% vs. 15.5%, p=0.062). This is because 60 patients (6.1%) were treated with R-miniCHOP [21] and more patients initially started R-CHOP at a reduced dose of doxorubicin (18.9%) and cyclophosphamide (12.4%) in this cohort than did patients in the PROCESS cohort. However, in the subsequent cycles, only 0.6% and 0.9% of patients experienced a dose reduction of > 20% for doxorubicin and cyclophosphamide, respectively. In contrast, fewer patients started treatment with a reduced dose of doxorubicin and cyclophosphamide (6.8% and 6.2%, respectively) in the PROCESS cohort, but more patients experienced a reduction of doxorubicin and cyclophosphamide (8.7% and 8.9%, respectively) in the subsequent cycles. Accordingly, the proportion of patients with ARDI of ≥ 80% did not differ between the two cohorts (73.2% in this cohort vs. 70.9% in the PROCESS cohort, p=0.353) (Table 3).
4. Risk factors for FN in patients treated with or without pegfilgrastim prophylaxis
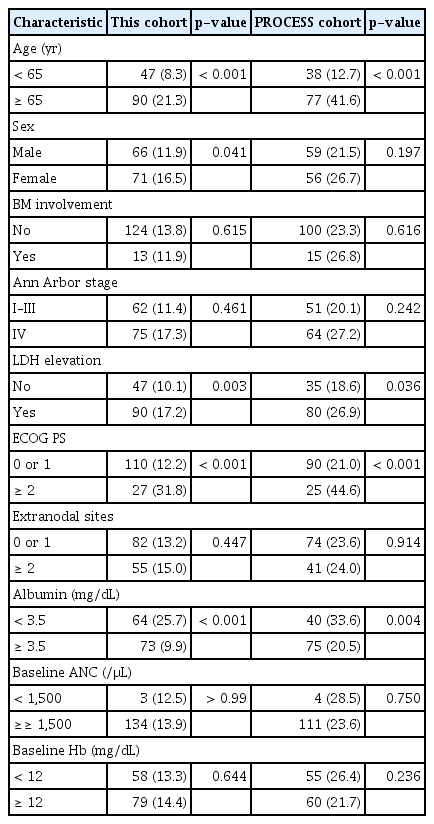
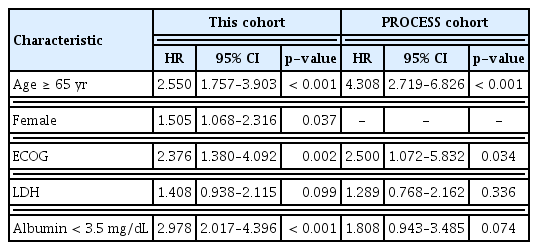
We analyzed the risk factors for FN according to the use of pegfilgrastim prophylaxis. In the PROCESS cohort, age ≥ 65 years, Eastern Cooperative Oncology Group (ECOG) performance status ≥ 2, lactate dehydrogenase (LDH) elevation, and albumin level < 3.5 mg/dL were significant risk factors for FN in the univariate analysis (p < 0.05) (Table 4). In the multivariate analysis, age (hazard ratio [HR], 4.308; 95% confidence interval [CI], 2.719 to 6.826) and performance status (HR, 2.500; 95% CI, 1.072 to 5.832) were significant (Table 5). In this cohort, age ≥ 65 years, female sex, ECOG performance status ≥ 2, LDH elevation, and albumin level < 3.5 mg/dL were significantly associated with FN in the univariate analysis. In the multivariate analysis, age ≥ 65 years (HR, 2.550; 95% CI, 2.719 to 6.826), female sex (HR, 1.505; 95% CI, 1.068 to 2.316), ECOG performance status ≥ 2 (HR, 2.376; 95% CI, 1.380 to 4.092), and albumin level < 3.5 mg/dL (HR, 2.987; 95% CI, 2.017 to 4.396) remained significant.
5. Treatment outcome and survival
The overall response rate with R-CHOP in this cohort was 90.9% (complete response, 80.6%; partial response, 10.3%), which was not different from that in the PROCESS cohort [18]. At the time of analysis, 707 patients (71.7%) who were being followed up were alive, with a median follow-up duration of 44 months. The four-year OS and PFS rates in this cohort were 73.9% and 69.4%, respectively. In the PROCESS cohort, 451 patients (93.0%) were available for full survival analysis, with median follow-up duration of 47 months for the survivors. We performed PSM to compare survival between the two cohorts. After PSM with the parameters of IPI and sex, the OS and PFS rated of 245 patients from each cohort were compared (S1 Table). The 4-year OS and PFS rates of the two cohorts after PSM were not significantly different (OS: 73.0% in this cohort vs. 71.9 in the PROCESS cohort, p=0.545; PFS: 69.5% in this cohort vs. 68.8% in the PROCESS cohort, p=0.616) (Fig. 3A and B). However, for patients aged ≥ 75 years, the 4-year OS and PFS rates of this cohort were higher than those of the PROCESS cohort (OS: 49.6% vs. 33.7%, p=0.032; PFS: 44.2% vs. 30.3% p=0.047) (Fig. 3C and D).
Discussion
The prophylactic effect of pegfilgrastim has not been fully evaluated throughout the cycles of standard R-CHOP in DLBCL patients as previous studies included heterogeneous disease groups (NHLs), diverse regimens (CHOP, R-CHOP, and others), use of pegfilgrastim only in the first cycle, or mixed use of G-CSF or pegfilgrastim [9,10,22–24]. In real-world practice, primary prophylaxis is not fully performed [13]. As pegfilgrastim prophylaxis has been available in Korea since 2014, we were able to compare the incidence of FN and treatment outcomes of DLBCL patients treated with R-CHOP between two cohorts collected during different time periods. Although this study was not a randomized trial, the two cohorts compared in this study were homogenous in terms of ethnicity, disease, treatment regimen, and other clinical characteristics. In addition, more than 90% of all cycles of R-CHOP were delivered with pegfilgrastim prophylaxis in this cohort, which was not given to the historical control cohort. Thus, we believe that the evidence provided by this study is valuable for evaluating the benefits of pegfilgrastim prophylaxis.
In this study, the proportion of patients who experienced FN throughout cycles of R-CHOP treatment was significantly lower than that in the PROCESS cohort (13.9% vs. 23.7%, p < 0.001) (Fig. 2). This was similar to the result of a previous study (16%) that retrospectively analyzed the incidence of FN with pegfilgrastim prophylaxis in aggressive NHLs [25]. As in previous studies, the incidence of FN was highest in the first cycle (8.3%) despite the use of pegfilgrastim prophylaxis [7,26]. Therefore, pegfilgrastim prophylaxis is essential for all patients in the first cycle of R-CHOP, and patients should be monitored around the 7th day of R-CHOP treatment when FN occurs most frequently. Although the overall incidence of FN significantly decreased in the subsequent cycles in both cohorts, continuous use of pegfilgrastim prophylaxis in this cohort reduced the incidence of FN by more than 50% compared to that in the PROCESS cohort. Subsequently, the incidence of TRM (3.2% vs. 5.6%, p=0.047) and infection-related deaths (1.8% vs. 4.5%, p=0.004) was significantly lower in this cohort than in the PROCESS cohort, which signifies a substantial benefit in the treatment of DLBCL patients.
In the risk factor analysis, age and performance status were consistently associated with the occurrence of FN in both cohorts, as in previous studies [8–10]. Even with pegfilgrastim prophylaxis, FN occurred in more than 20% of patients aged ≥ 65 years (21.3%), with poor performance (ECOG ≥ 2) (31.8%) and albumin level < 3.5 mg/dL (25.7%) in this cohort (Table 4). As pegfilgrastim prophylaxis is not sufficient for these patients, it is desirable to use antibiotic prophylaxis as well. In addition, those who experience FN should be considered at high risk for it in the subsequent cycles, because these patients tended to have multiple episodes in the subsequent cycles in both cohorts (32.8% in this cohort and 42.6% in the PROCESS cohort), even up to six events in six cycles.
In terms of treatment delivery, more patients received treatment on schedule in this cohort pegfilgrastim prophylaxis than in the PROCESS cohort (Table 3). However, as the median age of patients recruited in this cohort was 3 years higher than in the PROCESS cohort (62 years vs. 59 years), more patients started R-CHOP at a reduced dose in the former than in the latter. Therefore, the proportion of patients receiving ARDI of ≥ 80% did not differ between the two cohorts (Table 3). However, it is likely that ARDI could be increased by pegfilgrastim prophylaxis. This assumption is supported by a recent analysis from Japan, where pegfilgrastim prophylaxis improved dose delivery in elderly patients [24]. Given that reduced dose intensities have been associated with poor outcomes in most studies [27,28], maintaining dose intensity with pegfilgrastim prophylaxis may improve overall treatment outcomes.
As the population continues to age, increased number of elderly patients need to be treated for lymphoma [29]. Therefore, the treatment of elderly patients with DLBCL, for whom cytotoxic R-CHOP is still the standard therapy, is becoming very important. A recent meta-analysis showed that unlike in younger patients, dose intensity is not strongly correlated with better survival in elderly patients with DLBCL (≥ 80 years) due to higher TRM with higher dose intensity [27]. Therefore, finding a balance between treatment intensity and toxicity is the most important factor in treating elderly patients. From this point of view, prevention of FN is crucial. In this study, more elderly patients started treatment with a lower dose of chemotherapy than in the previous cohort since the introduction of R-miniCHOP in 2011 [21]. The incidence of TRM and infection-related death among patients aged ≥ 75 years in this cohort was significantly lower than that in the PROCESS cohort with the prophylactic effect of pegfilgratsim (Table 2), which improved the OS rate of patients age ≥ 75 years in this cohort compared to that in the PROCESS cohort (Fig. 3B).
Based on the findings of this study and previous studies, the benefits of pegfilgrastim primary prophylaxis can be summarized as follows: (1) it reduces the incidence of FN and need for hospitalization [17,23,25]; (2) it provides better dose delivery [24,25]; (3) it is convenient as only a single injection is required and is more cost-effective compared to secondary prophylaxis, daily use of G-CSF, or treatment of FN [4,23,30]; and (4) it is associated with fewer infection-related deaths and better survival outcomes, especially in elderly DLBCL patients. Although OS benefit was not observed in the entire group, the current study supports more active use of pegfilgrastim prophylaxis in DLBCL patients treated with R-CHOP.
In conclusion, primary prophylaxis with pegfilgrastim significantly reduced the incidence of FN and infection-related death in DLBCL patients treated with R-CHOP, and it improved OS in patients aged ≥ 75 years.
Electronic Supplementary Material
Supplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
Notes
Ethical Statement
The protocol was reviewed and approved by the institutional review board of each participating center, and all patients provided written informed consent before treatment initiation; Gachon University Gil Medical Center: GCIRB2015-74, Gyeongsang National University Hospital: GNUH 2015-02-012, Dongsan Medical Center: DSMC 2015-03-015, Korea University Anam Hospital: ED15024(AN15024-001), Kosin University Gospel Hospital: KUGH 2017-09-008, National Cancer Center: NCC 2015-0091, Dong-A University Medical Center: DMC 15-037, Pusan National University Hospital: H-1701-011-051, Samsung Medical Center: SMC 2014-07-181, Seoul National University Hospital: H-1504-119-667, Asan Medical Center: S2015-0302-0001, Soonchunhyang University Hospital: SCHUH 2015-05-007, Soonchunhyang University Bucheon Hospital: SCHBC 2015-07-008, Wonju Severance Christian Hospital: CR315002-002, Ajou University Hospital: AJIRB-MED-OBS-14-254, Yeungnam University Medical Center: YUMC 2015-03-016, Korea Cancer Center Hospital: K-1409-001-001, Ulsan University Hospital: UUH 2015-11-007, Inje University Sanggye Paik Hospital: SGPAIK 2015-06-002, Inje University Ilsan Paik Hospital: ISPAIK 2015-07-002, Inje University Busan Paik Hospital: BS 2015-0110, Jeonbuk National University Hospital: CUH 2015-02-034, Chonnam National University Hwasun Hospital: TMP-2015-023, Chung-Ang University Hospital: C2015048(1506), Chungnam National University Hospital: CNUH 2015-10-060, Chungbuk National University Hospital: CBNUH 2015-03-006, Hallym University Sacred Heart Hospital: HUH 2015-I043.
Author Contributions
Conceived and designed the analysis: Jeong SH, Kim SJ, Kim WS.
Collected the data: Jeong SH, Kim SJ, Yoon DH, Park Y, Kang HJ, Koh Y, Lee GW, Lee WS, Yang DH, Do YR, Kim MK, Yoo KH, Choi YS, Yun HJ, Yi JH, Jo JC, Eom HS, Kwak JY, Shin HJ, Park BB, Hyun SY, Yi SY, Kwon JH, Oh SY, Kim HJ, Sohn BS, Won JH, Kim SH, Lee HS, Suh C, Kim WS.
Contributed data or analysis tools: Jeong SH, Kim SJ, Choi YS, Kim WS.
Performed the analysis: Jeong SH, Kim SJ, Kim WS.
Wrote the paper: Jeong SH, Kim SJ.
Conflicts of Interest
This study was supported by the Kyowa Kirin Korea Co., Ltd.
Acknowledgements
This study was supported by the Consortium for Improving Survival of Lymphoma (CISL).