Adherence to the Recommended Intake of Calcium and Colorectal Cancer Risk in the HEXA Study
Article information
Abstract
Purpose
Dietary calcium intake has been suggested to be protective against the development of colorectal cancer. The mean dietary calcium intake of Koreans is 490 mg/day, which is far below the recommended calcium intake of 700-800 mg/day. In this study, we explored the relationship between dietary calcium intake and colorectal cancer development in Koreans with relatively low calcium intake compared with individuals in Western countries.
Materials and Methods
The Health Examinees Study, a large-scale genomic community-based prospective cohort study, was designed to identify the general characteristics of major chronic diseases in Koreans. A total of 119,501 participants aged 40-69 years recruited between 2004 and 2013 were included in this analysis. The calcium intake level was categorized using the Dietary Reference Intakes for Koreans (KDRIs). The Cox proportional hazards regression model was used to estimate the hazard ratio (HR) and the corresponding 95% confidence intervals (CIs) for colorectal cancer risk, adjusting for potential confounders.
Results
In the multivariable-adjusted model, compared with the group that consumed less than the recommended amount of calcium, the group that consumed more than the recommended intake of calcium showed a significant reduction in the risk of colorectal cancer in women. (HR, 0.54; 95% CI, 0.31 to 0.95). Among men, however, no significant association was observed between dietary calcium intake and colorectal cancer risk (HR, 0.89; 95% CI, 0.54 to 1.45).
Conclusion
Korean women who adhere to the recommended intake of calcium showed a reduced risk of colorectal cancer.
Introduction
Colorectal cancer is the third most common cancer globally, and the burden of disease from colorectal cancer is expected to increase by 60% by 2030, with 2.2 million more patients worldwide [1]. In Korea, colorectal cancer is the second most commonly diagnosed cancer in men and the third most common cancer in women [2]. A systematic review of epidemiological studies by the World Cancer Research Fund (WCRF) published in 2011 classified dietary calcium as a probable protective factor against colorectal cancer development [3]. The updated 2017 WCRF report grouped dairy products including calcium and calcium supplements as probable protective factors against colorectal cancer development [4]. Although there is inconsistency in the protective effect of calcium at high intake levels, a low intake of calcium has consistently been associated with a reduced risk of colorectal cancer [5-7].
Korea established the 2015 Dietary Reference Intakes for Koreans through the National Nutrition Management Act. The established reference levels were based on internationally published scientific evidence and included a total of 36 nutrients, including calcium. According to the 2018 National Health and Nutrition Survey, the average daily intake of calcium in Korean adults aged 19 and older was 514.3 mg [8], which was far below the recommended calcium intake of 700-800 mg. The average daily intake of calcium among the U.S. population is 934 mg, and the average daily intake of dietary calcium in northern European countries exceeds 1,000 mg [9]. In the current study, we explored whether the recommended calcium intake standard helps lower the risk of colorectal cancer in a Korean population using a large-scale cohort study.
Materials and Methods
1. Study population
The Health Examinees Study (HEXA), part of the Korean Genome and Epidemiology Study (KoGES), is a large-scale community-based prospective genomic cohort study. HEXA was created to investigate the causes of major chronic diseases in Koreans, including cancer. A total of 169,718 men and women aged 40 to 69 were selected and recruited using strict standardized study protocols by the Korean Centers for Disease Control and Prevention from 2004 to 2013 at 38 hospitals and local health examination centers. More information about the HEXA study, such as its rationale and baseline population characteristics, has been previously published [10].
The HEXA-G cohort was based on the HEXA study and was created by grouping individuals from participating sites (e.g., health examination centers and training hospitals) who met additional eligibility criteria. Exclusion criteria for the HEXA-G cohort were reported in detail in a previous study [11]. Of the 139,342 members of the HEXA-G cohort, 19,841 were excluded for the following reasons: (1) individuals (n=11,303) who did not consent to link the secondary data such as cancer registry, (2) individuals (n=6,104) who were diagnosed with cancer before entry date, (3) individuals (n=1,557) without information related to their calcium intake, and (4) individuals (n=877) with daily energy intake < 500 kcal or ≥ 4,000 kcal. A total of 119,501 subjects (40,943 men and 78,558 women) was included in the final analysis.
2. Assessment of calcium intake and other factors
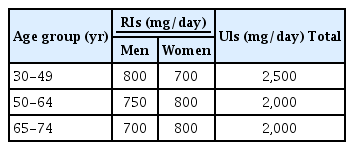
The participants’ information was collected at baseline by well-trained staff using a structured questionnaire; data included general demographic characteristics, a dietary survey, smoking status, alcohol consumption habits, physical activity, and disease history. A 106-food item semi-quantitative food frequency questionnaire (SQFFQ) developed by the Korea Center for Disease Control and Prevention was used to estimate individuals’ usual food intake habits over the past 12 months. The Validity and Reliability of the SQFFQ were reported previously [12]. Daily calcium and calorie intake were calculated via a food composition table developed by the Korean Health and Industry of Development Institute [13]. The standard calcium intake was based on the 2015 Dietary Reference Intakes for Koreans, which were established through the National Nutrition Management Act. Recommended calcium intake levels by age and sex are shown in Table 1. Calcium intake through supplements was not considered.
3. Identification of colorectal cancer cases
Incident colorectal cancer cases were identified through linkage with the Korea Central Cancer Registry data through the end of December 2014. Data linkage was requested by the Korean Centers for Disease Control and Prevention to Korea Central Cancer Registry based on the informed consent obtained from the study participants. The personal identification numbers of participants who agreed on the linkage to the secondary data such as cancer registry, health insurance data, and mortality database were used for the linkage. The completeness, which is defined as the extent to which all the incidence cancers occurring in a target population are included in the registry database, of the Korea Central Cancer Registry in 2014 was estimated at 97.8% based on the method using the proportion of death certificate only cases [14]. Colorectal cancer cases were defined as either colon cancer (C18-C19) or rectal cancer (C20) according to the International Classification of Diseases, 10th revision.
4. Statistical analysis
Cox proportional hazards regression model (using age at time scale) were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) to investigate the association between daily calcium intake and incidence of colorectal cancer. We used individual age as a time scale, and entry time was age at cohort recruitment. Age at exit time was whichever of the following occurred first: diagnosis of colorectal cancer, the end of follow-up (December 31, 2014), or the date of death. Calcium intake level was categorized by recommended intake amount for the corresponding age group or in 200 mg/day increments for comparison with the continuous update project (CPU) issued by the WCRF. Calcium intakes were adjusted for total individual energy intakes using the residual method. We have additionally adjusted the risk factors for colorectal cancer as assessed at baseline. Potential confounding variables investigated after review of the literature included: education level (less than high school, high school, college or above, missing), smoking status (non-smoker, ex-smoker, current smoker, and missing), body mass index (<18.5 kg/m2, 18.5-22.9 kg/m2, 23-24.9 kg/m2, ≥ 25 kg/m2, and missing), alcohol intake (non-drinkers, ex-drinkers, current drinkers, and missing), physical activity (none, < 210 min/wk, ≥ 210 min/wk, and missing), total energy intake (quartiles), red meat intake (quartiles), and processed meat intake (0 g, > 0 g).
Results
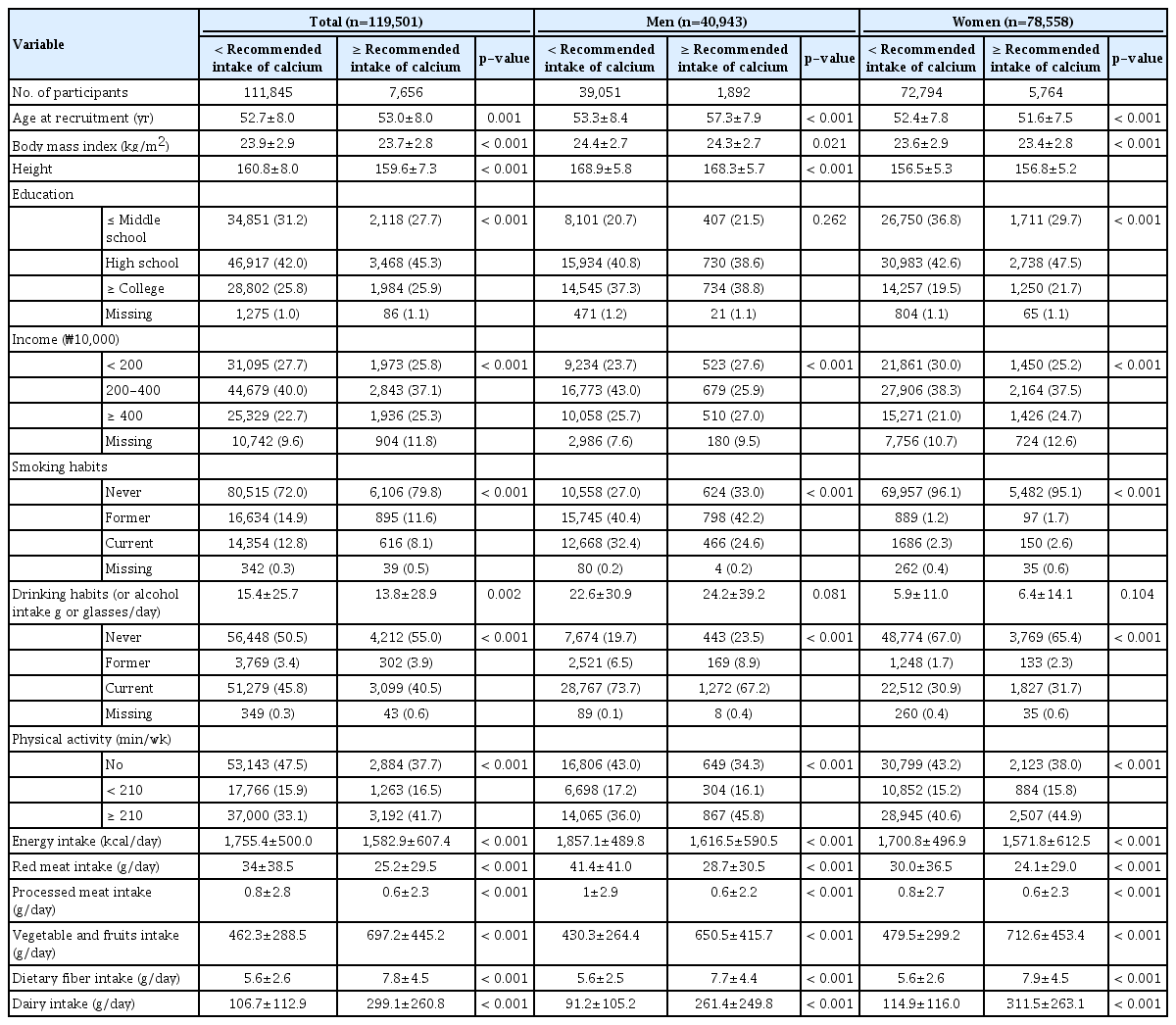
During a mean follow-up of 5.4 years (647,612 person-years), there were 635 cases of colorectal cancer, 318 in men and 317 in women. The general characteristics of the participants according to adherence to the recommended intake of calcium are presented in Table 2. The findings showed that men who consumed more than the recommended intake of calcium tended to be older, whereas women who consumed more than the recommended intake of calcium were younger than their counterparts. Both the men and women who consumed more than the recommended calcium intake were highly educated; exercised more; had lower total energy intake; consumed less red and processed meats; and consumed more fruits, vegetables, and dairy products than those who consumed less than the recommended calcium intake.
Table 3 shows the risk of colorectal cancer with adherence to the recommended calcium intake. Women who consumed more than the recommended amount of calcium had a 46% lower risk of colorectal cancer (HR, 0.54; 95% CI, 0.31 to 0.95) compared with women who consumed less than the recommended amount of calcium. However, no significant differences in risk were found in men. Although the results for the stratified analysis by sex were not statistically significant, a reduced risk for colon cancer was observed in women and men combined for each 200 mg/day increment in calcium intake (HR, 0.90; 95% CI, 0.81 to 0.99).
Discussion
In this large-scale prospective cohort study of Koreans, we found that women who consumed more than the daily recommended amount of calcium had a reduced risk of colorectal cancer compared with women who did not meet the dietary recommendation level.
There are no previous studies specifically examining the association between adherence to the recommended intake of calcium and colorectal cancer risk, but many previous studies have found that calcium intake is beneficial for the prevention of colorectal cancer. In the results of the most recent meta-analysis, women with higher dietary calcium intake were found to have a 30 percent reduction in colorectal cancer risk [15]. In the dose response meta analyses of the prospective observational studies published in 2014, each 300 mg/day increase in total calcium intake showed an approximately 10% reduction in colorectal cancer risk [7]. Case-control studies from Korea [6], Japan [16], China [17] and two women cohorts from the European Prospective Investigation into Cancer and Nutrition (EPIC) study [18] also reached the same conclusion, while other studies [19-22] have shown no association between colorectal cancer risk and high dietary calcium intake. The variance in these findings is likely due to differences in intake of calcium-based foods resulting from differences in food cultures.
The results of our study are similar to previously published findings that dietary calcium intake lowers the risk of colorectal cancer, although some caution is advised in interpreting these results. First, we set the standard of calcium intake as the recommended daily intake of calcium, while most of the literature is based on quartiles, quintiles, or mean values. Second, average calcium intake and dietary calcium sources differ between Koreans and individuals in Western countries. In our study, median energy-adjusted calcium intake was 388.4 mg/day in men and 422.1 mg/day in women, which were both lower than the intake level of Western populations, where the average daily calcium intake is more than 900 mg [9]. Since the typical Korean diet consists of bap (steamed rice), kuk, or chigae (broth, stew), banchan (side dishes) and kimchi, Koreans usually obtain their dietary calcium from kimchi, anchovies, tofu and radish leaves [23], whereas milk and dairy products are the most significant dietary sources of calcium for individuals in Western countries. Third, calcium metabolism varies by race, as genetic differences, calcium absorption, and bioavailability differ by race [24].
Several potential mechanisms have been proposed to explain how dietary calcium intake is beneficial for the prevention of colorectal cancer. Calcium binds with free ionized fatty acids and secondary bile acids to neutralize carcinogenesis [13]. Additionally, in vitro studies have shown that calcium inhibits the progression of cancer by controlling the balance between the proliferation, differentiation, and apoptosis of colonic epithelial cells; through the activation of calcium-sensing receptors; and through the promotion of E-cadherin signals [25,26].
In our study, significant results were found only in women, demonstrating gender differences in outcomes. The underlying mechanisms of gender differences in our research are not clearly known, but there are several possibilities to consider. The absorption of calcium is affected by age, sex, race, pregnancy, lactation, and menopausal status [27]. Previous studies have shown that exposure to estrogen [28], the use of oral contraception [29] and hormone replacement therapy [30] have decreased colorectal cancer risk. Additionally, in our study, women were found to consume more dairy products and calcium than men. In general, women tend to know more about the health benefits of calcium because they are in charge of buying and cooking food in Korean culture [31].
In conjunction with the large population size and prospective cohort design, the diagnosis of cancer in this cohort was confirmed by the Korea Central Registry; the high accuracy of colorectal cancer diagnosis, therefore, is an additional strength of this study. Additionally, the present study is the first exploration of the association between adherence to the recommended intake of calcium and the risk of colorectal cancer in the Korean population, where the food sources of calcium may differ from Western countries. Despite the previously mentioned advantages, there are also some limitations to consider in this study. First, the possibility of some residual and unmeasured confounding has not been eliminated. Thus, we adjusted for education level, smoking status, BMI, alcohol intake, physical activity, total energy intake, and red and processed meat consumption that we have identified as potential confounders in our analysis. Second, we did not consider calcium supplements because we could not obtain detailed information related to calcium supplement intake. Third, further analysis of the dietary calcium sources was not performed because a detailed database was not available.
In conclusion, our results suggest that compliance with recommended calcium intake lowers the risk of colorectal cancer in women. Further research is required to examine improvements in public health through a balanced diet by reviewing adherence to the recommended intake levels of calcium and colorectal cancer risks.
Notes
Ethical Statement
The protocol of the present study including the data linkage to the cancer registry was approved by the Ethics Committee of the Korean Health and Genomic Study of the Korean National Institute of Health (IRB number 2014-08-02-3C-A) and the Seoul National University Hospital, Seoul, Korea (IRB No. E-2002-003-1097). All participants were given a detailed description of the study, and written informed consent was collected from all participants.
Author Contributions
Conceived and designed the analysis: Lee J, Shin A, Choi JY, Kang D.
Collected the data: Lee JK, Kang D, Choi JY, Shin A.
Contributed data or analysis tools: Lee J, Shin A.
Performed the analysis: Lee J, Shin A.
Wrote the paper: Lee J.
Conflicts of Interest
Conflicts of interest relevant to this article was not reported.
Acknowledgements
Cancer Data in this study were from Korea Central Cancer Registry Database, National Cancer Center).
This study was supported by the National Research Foundation of Korea, No. 2017R1A2B4009233; and the Research of Korea Centers for Disease Control and Prevention. No. 2004-E71004-00; 2005-E71011-00; 2005-E71009-00; 2006-E71001-00; 2006-E71004-00; 2006-E71010-00; 2006E71003-00; 2007-E71004-00; 2007-E71006-00; 2008-E7100600; 2008-E71008-00; 2009-E71009-00; 2010-E71006-00; 2011E71006-00; 2012-E71001-00; 2013-E71009-00; 2018-P7106-00).