Long-Term Outcome of Definitive Radiotherapy for Early Glottic Cancer: Prognostic Factors and Patterns of Local Failure
Article information
Abstract
Purpose
This study evaluates the long-term results of definitive radiotherapy (RT) for early glottic cancer. Clinical and treatment factors related to local control and patterns of failure are analyzed.
Materials and Methods
We retrospectively reviewed 222 patients with T1-2N0 squamous cell carcinoma of the glottic larynx treated with definitive RT from 1981 to 2010. None of the patients received elective nodal RT or combined chemotherapy. The median total RT dose was 66 Gy. The daily fraction size was < 2.5 Gy in 69% and 2.5 Gy in 31% of patients. The RT field extended from the hyoid bone to the cricoid cartilage.
Results
The median age was 60 years, and 155 patients (70%) had T1 disease. The 5-year rates of local recurrence-free survival (LRFS) and ultimate LRFS with voice preservation were 87.8% and 90.3%, respectively. T2 (hazard ratio [HR], 2.30; 95% confidence interval [CI], 1.08 to 4.94) and anterior commissural involvement (HR, 3.37; 95% CI, 1.62 to 7.02) were significant prognostic factors for LRFS. In 34 patients with local recurrence, tumors recurred in the ipsilateral vocal cord in 28 patients. There were no contralateral vocal cord recurrences. Most acute complications included grade 1-2 dysphagia and/or hoarseness. There was no grade 3 or greater chronic toxicity.
Conclusion
Definitive RT achieved a high cure rate, voice preservation, and tolerable toxicity in early glottic cancer. T2 stage and anterior commissural involvement were prognostic factors for local control. Further optimization of the RT method is needed to reduce the risk of ipsilateral tumor recurrence.
Introduction
Squamous cell carcinoma of the glottis is the most common form of laryngeal cancer. Tumors arising on true vocal cords result in hoarseness at an early stage, and the incidence of positive lymph nodes for T1-2 glottic cancer is low due to minimal lymphatic drainage [1]. Based on clinical presentations and a favorable prognosis, the aim of therapeutic management is not only tumor control but also preservation of laryngeal function [2].
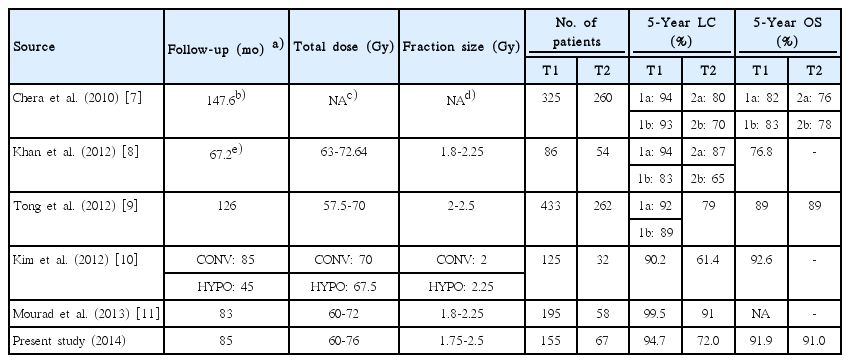
Radiotherapy (RT) and CO2 laser excision are the first choice of treatments for early glottic cancer [3]. Although both modalities produce similar outcomes, RT is the preferred option for improved voice quality, especially in cases of bulky tumors, infiltrative growth pattern, and tumors with anterior commissural involvement [4,5]. The historical data reported 5-year overall survival rates of 80%-85% and local control rate of 79% [1,6]. In current retrospective studies, the 5-year local control rates were 85%-95% for T1 and 70%-80% for T2 with definitive RT, and cause-specific survival rates were usually higher than 90% [7-11]. However, the total RT dose, fractionation scheme, and target volume have been dependent on the institution’s policy.
The purpose of this study is to present our long-term results of definitive RT for early-stage squamous cell carcinoma of the glottis. We analyzed the prognostic factors that had a significant impact on local tumor control and evaluated patterns of failure.
Materials and Methods
1. Patients
After receiving an approval from the Institutional Review Board, we reviewed 438 patients with malignancy in the glottic larynx referred to our clinic between January 1981 and December 2010. Two hundred twenty-two consecutive cases of T1N0 or T2N0 glottic cancer treated with definitive RT were identified. In our institution, definitive RT has been the mainstay in the treatment of these patients. Patients with synchronous primary cancer and with medical history of prior surgery of the neck or chemotherapy were excluded. Squamous cell carcinoma of the glottis was confirmed by biopsy in all patients. The American Joint Committee on Cancer (AJCC) staging system used in this study was T1 for a tumor confined to a single (T1a) vocal cord or both (T1b) vocal cords, and T2 for a tumor with supraglottic or subglottic extension, with or without impaired vocal cord mobility. Old cases of T2a and T2b before applying the sixth version of the AJCC’s staging system were re-staged. A physical examination with laryngoscopy was used for the staging procedure. Computed tomography, magnetic resonance imaging, and positron emission tomography-computed tomography were not routinely performed.
2. Treatment and follow-up
No patients received combined chemotherapy or elective nodal irradiation. RT was delivered using two-dimensional (2D) conventional RT until 2005, and the three-dimensional (3D) conformal technique was used since 2006. The beam energy consisted of 60Co and 4-MV or 6-MV photons, and 60Co was used until 1992. Patients were immobilized in a supine position with a thermoplastic mask. Right/left or right anterior oblique/left anterior oblique beams were used in 2D conventional RT, and the field size ranged from 20 to 42 cm2 based on the anatomy and extent of the disease. In the 3D conformal technique, the clinical tumor volume (CTV) was defined as the whole larynx, and the planning target volume was an expansion of CTV by 0.5 cm. The borders of the RT field were (1) superior: lower level of hyoid bone, (2) inferior: lower margin of cricoid cartilage, (3) anterior: beyond the skin surface, and (4) posterior: anterior border of the vertebral body of cervical spine. Paired wedge filters of 15º, 30º, or 45º were used to improve dose homogeneity.
The median total RT dose was 66 Gy (range, 60 to 76 Gy). T1 and T2 patients received a median of 65 Gy (range, 60 to 76 Gy) and 67 Gy (range, 60 to 70.75 Gy), respectively. The fraction size ranged from 1.75 to 2 Gy until December 1998, and 2.5 Gy was administered since January 1999. Fifty-nine patients (38.1%) with T1 and 11 (16.4%) with T2 disease were treated with 2.5 Gy/fx. The median overall treatment time was 48.0 days (range, 27.9 to 77.1 days) for T1 and 53.1 days (range, 32.1 to 69.0 days) for T2 disease. All patients were treated once daily with five fractions per week.
As patients were treated with different doses and fractionation schemes, the biologically effective dose (BED) for tumors was calculated by considering tumor proliferation based on a linear quadratic model. The equation used in this study was as follows.
The definition of BED is the total dose multiplied by relative effectiveness, which is the first part of the above equation. The second part consists of time-dependent factors that involve the compensatory effect of tumor repopulation during the treatment. The definitions of basic parameters necessary for the calculations are listed below.
1) n: number of fractions.
2) d: dose per fraction (Gy).
3) α/β: the dose at which the linear and quadratic portions of the cell killing are equal in radiation biology. The value represents the ratio of intrinsic radiosensitivity in the specific cells and tissues. We assumed 15 for the value based on Tong et al. [9].
4) α: the cell killing per Gy on a log-linear plot of the linear quadratic model. The parameter indicates the average intrinsic radiosensitivity. The range of 0.3-0.35/Gy has been accepted for most epithelial tumors [12], and 0.35/Gy was used in the present study.
5) T (day): the overall treatment time of irradiation. The prolongation of the parameter is positively related to increased tumor repopulation.
6) Tk (day): the kick-off time, denoting the time between the start of treatment and the initiation of accelerated proliferation during the treatment. We assumed 28 days for human head and neck tumors [13].
7) Tp (day): the potential doubling time, representing the average doubling time of cancer cells during the treatment. We adopted 3 days for human head and neck tumors [13].
After the completion of RT, a radiation oncologist and/or otolaryngologist conducted regular follow-up evaluations. History taking and physical examination with laryngoscopy were performed in an outpatient clinic. Imaging studies were not routinely performed. The pre- and post-RT change in voice quality were recorded as ‘aggravated, ditto, and improved’ in a self-reported fashion. Acute and late toxicities were assessed according to Common Terminology Criteria for Adverse Events ver. 4.0.
3. Statistical analysis
Overall survival (OS) was defined as the interval from the start date of RT to the date of death. Local recurrence-free survival (LRFS) was defined as the interval from the start date of RT to the date of the diagnosis of local tumor recurrence. Kaplan-Meier analysis was used to estimate the OS and LRFS rates. The survival differences according to clinicopathological factors were evaluated by a two-sided log-rank test. The results of the analyses were declared statistically significant if the p-value was less than 0.05. Cox proportional hazards regression was used in multivariate analyses. Statistical analyses were performed with SPSS ver. 20.0 software (IBM Corp., Armonk, NY).
Results
1. Clinical characteristics
Patient, tumor, and treatment characteristics are listed in Table 1. The median age was 60 years (range, 35 to 86 years), with male preponderance (male:female=43.4:1). T1a and T1b diseases were observed in 122 (55%) and 33 (15%) patients, respectively, and 56 (25%) patients had tumors with anterior commissural involvement. With the median BED15 of 74.67 Gy15 (range, 67.88 to 85.96 Gy15), a total BED15 ≥ 74.67 Gy15 was delivered to 107 patients (48%), and the fraction size was < 1.8 Gy in 11 (5%), 1.8 Gy in 115 (52%), 2 Gy in 26 (12%), and 2.5 Gy in 70 (31%) patients. The median overall treatment time was 50 days (range, 28 to 77 days). RT with the 2D bilateral technique was delivered to 199 patients (90%). The photon energy of 4 MV or 6 MV was used in 129 (58%) patients.
2. Local control and related predictive factors
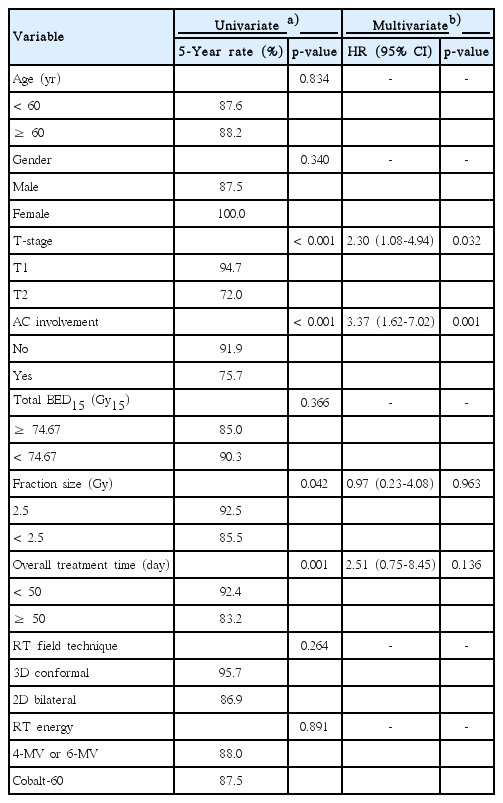
The median duration of follow-up was 85.2 months (range, 11.0 to 313.1 months). The 5-year OS rate was 91.7%. The 5-year rates of LRFS and ultimate LRFS with voice preservation were 87.8% and 90.3%, respectively (Fig. 1A and B). In the univariate analysis for LRFS, T-stage (T1 vs. T2, p < 0.001), anterior commissural involvement (no vs. yes, p < 0.001), RT fraction size (2.5 Gy vs. < 2.5 Gy, p=0.042), and overall treatment time (< 50 days vs. ≥ 50 days, p=0.001) were statistically significant (Table 2). In the multivariate analysis, T2 disease (hazard ratio [HR], 2.30; 95% confidence interval [CI], 1.08 to 4.94) and anterior commissural involvement (HR, 3.37; 95% CI, 1.62 to 7.02) were significantly poor prognostic factors. The 5-year LRFS rates were 94.7% and 72.0% for T1 and T2 disease, respectively (Fig. 2A), and 91.9% and 75.7% for tumors without and with anterior commissural involvement, respectively (Fig. 2B). The 5-year LRFS rates were 92.5% and 85.5% for an RT fraction size of 2.5 Gy and < 2.5 Gy, respectively (Fig. 3A), and 92.4% and 83.2% for overall treatment time of < 50 days and ≥ 50 days, respectively (Fig. 3B).
Kaplan-Meier curve for local recurrence-free survival (A) and ultimate local recurrence-free survival (B) with voice preservation.
Local recurrence-free survival according to T-stage (T1 vs. T2, p < 0.001) (A) and anterior commissural involvement (no vs. yes, p < 0.001) (B) by Kaplan-Meier analyses. AC, anterior commissure.
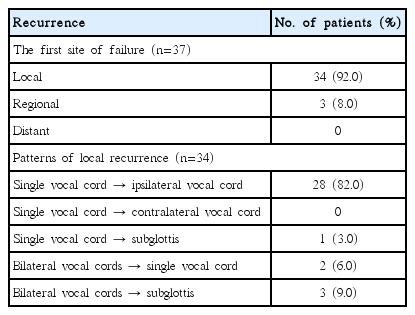
3. Patterns of failure
At the time of analysis, tumor relapse was reported in 37 patients (17%). Table 3 shows the initial patterns of failure in the study population. The treatment failure involved local recurrences in 34 patients, and the median time to relapse was 1.4 years (range, 0.3 to 13.2 years). Three patients had regional recurrences, and the median time to recurrence was 4.0 years (range, 2.5 to 4.3 years). The initial treatment failure did not include distant metastasis in any of the patients. In patients with local relapse, 28 had ipsilateral vocal cord recurrences. There were no contralateral vocal cord recurrences. Four patients had recurred tumors in the area of the subglottis.
4. Salvage treatment and causes of death
In the 40 patients who underwent salvage treatment, salvage surgery (total laryngectomy, partial laryngectomy, laryngofissure and cordectomy, laser microsurgery, or neck node dissection) was performed in 37. Other salvage treatment modalities included concurrent chemoradiation therapy and chemotherapy. Twelve patients received the second salvage operations due to further locoregional tumor progression. Distant metastases were observed in five patients following the salvage surgery. After the salvage treatment had finished, 19 patients experienced loss of voice. Four patients complained of aggravation of voice quality, and 16 reported an improved status or no change.
At the time of analysis, 88 patients had died. Death events due to aggravation of glottic cancer and other malignancies were observed in 16 and 15 patients, respectively. Forty-seven patients had died of old age or other medical comorbidities. Among the patients who received salvage treatment, 16 had died. There were seven and three events of cause-specific death and death from other malignancies, respectively.
5. Treatment toxicity
Most patients reported grade 1-2 dysphagia and hoarseness during the treatment. One hundred eighty-one (82%) patients reported an improvement of voice quality after the completion of RT. Two and nine patients reported acute toxicities of grade 3 dysphagia and hoarseness, respectively, with symptoms subsiding within several months. Grade 2 chronic laryngitis or laryngeal edema was observed in eight patients. Grade 3 or higher chronic toxicities were not reported, and no patient required permanent tracheostomy due to persistent laryngeal edema.
Discussion
The primary aim of early glottic cancer treatment is to eradicate the tumor with preservation of the larynx. The maintenance of voice quality and swallowing function after the treatment is also very important. As there have been no randomized trials to compare conservative surgery with RT, the evaluation of treatment outcomes has been mainly based on retrospective studies. The present study is also a retrospective analysis of definitive RT for T1-2N0 glottic cancer. However, we analyzed the long-term results of large-scale data from a single institution.
As shown in Table 4, the 5-year rates of LRFS and OS in the present study are comparable to the results of other series [7-11]. In the multivariate analysis, T2 disease and anterior commissural involvement were independent poor prognostic factors for local control. This result is consistent with that of other retrospective studies [14-17].
Tumors at the anterior commissure tend to spread into the thyroid cartilage, resulting in early progression with partial cartilaginous or extra-laryngeal invasion. Marshak et al. [14] reported that the 5-year local control rates of tumors, with and without anterior commissural involvement, were 74% and 89% (p=0.0027), respectively. Tong et al. [15] demonstrated that underestimation of the extent of the tumor due to insufficient radiological imaging and underdosage at the air-tissue interface could result in a negative impact of anterior commissural involvement on tumor control. Although there is still some controversy [8,18], we suggest that anterior commissural involvement should be considered for routine staging systems.
In previous studies, T2 stage was independently associated with a lower cure rate [16,17]. A retrospective study which analyzed Tis-T2 tumors identified that T2 disease was the only independently significant factor [16]. Burke et al. [17] demonstrated that T-stage was significant in local control (p=0.0009) and underlined the treatment-related implications in T2 tumors with inferior tumor control. Although both RT and CO2 laser excision are the standard management options, conservative surgery cannot guarantee voice quality in T2 or bulky tumors. To enhance the cure rate of early glottic cancer, accurate staging and discussion on optimal therapeutic modality are needed.
Previous studies tried to find out the clinical efficacy of a larger fraction size [19,20]. Decreasing the accelerated repopulation of cancer cells and shortening the overall treatment time are the main objectives. In a prospective randomized study, Yamazaki et al. [19] reported superior local control with 2.25 Gy/fx compared with 2 Gy/fx. More recently, Moon et al. [20] designed a randomized trial and demonstrated that local progression-free survival of a group that received 2.25 Gy/fx was not inferior to that of a conventional arm. In our institution, the dose per fraction for early glottic cancer was 1.8 to 2.0 Gy/fx until December 1998, and treatment with 2.5 Gy/fx was started from January 1999. The absence of significant differences in the multivariate analysis according to fraction size (2.5 Gy vs. < 2.5 Gy) and overall treatment time (< 50 days vs. ≥ 50 days) may be attributed to an insufficient follow-up duration of hypofractionation in comparison with the conventional treatment. Therefore, a longer follow-up is needed to assess the treatment efficacy of the hypofractionation strategy.
This study calculated the tumor BED (Gy15) considering both total RT dose and time-related factors. The local tumor control was not significantly different according to the value of BED ≥ 74.67 Gy15 or < 74.67 Gy15, and altering the cutoff values also did not result in statistically significant differences. Although the level of tumor BED that is adequate to kill laryngeal tumor cells has not been definitively established, Tong et al. [9] demonstrated that total BED15 less than 65 Gy15was related to poorer tumor control. Considering that the lowest value of BED was 67.88 Gy15 in the present study, we suggest that total BED15 was sufficiently high and a differential tumoricidal effect of definitive RT could not be verified.
With regard to patterns of local failure, most recurrent tumors occurred in the ipsilateral vocal cord, with no isolated contralateral recurrence observed. Therefore, we suggest that the prevention of ipsilateral vocal cord recurrence is important in early glottic cancer. As we treated the whole larynx in each case, the lack of contralateral failure could be due to the fact that the contralateral vocal cord was treated. However, the poor eradication of tumors at the ipsilateral site was noticeable.
More recently, dosimetric studies have reported the feasibility of the ipsilateral vocal cord intensity-modulated RT (IMRT), mainly in T1 disease [21-23]. Although the sparing of the organs-at-risk (contralateral vocal cord, arytenoids, swallowing muscles, carotid arteries, thyroid gland, and spinal cord) is the main advantage of the technique [21], the problems of tumor motion, hot spots, and contouring errors have limited the use of IMRT in early glottic cancer [22]. In a comparative study regarding IMRT and 2D RT planning [23], IMRT using image-guided technique resulted in comparable target coverage with significant reduction of radiation dose in normal tissues. The authors suggested the potential for better functional preservation with the equivalent tumor control in IMRT.
As mentioned in the present study, the poorer treatment outcomes of T2 disease and tumors with anterior commissural involvement remain unresolved. An earlier study demonstrated the importance of shorter overall treatment time and a larger fraction size to improve local control in T2 tumors [24]. In a recent study on early glottic tumors with anterior commissural involvement [15], higher tumor BED and a larger fraction size were significantly positively associated with better local control, and the authors suggested a negative impact of underdosage at the air-tissue interface on the tumor control in such patients. Since the increase in tumor dose is limited due to the normal tissue toxicities, the highly conformal RT technique can be beneficial in such high-risk subgroups. However, previous IMRT studies have focused on small or T1 vocal cord tumors. Further analyses are necessary to investigate the feasibility of the new RT method in T2 disease or tumors with anterior commissural involvement.
Researchers at the University of Texas Southwestern performed a phase I study of unilateral vocal cord RT for T1a glottic cancer (Choy H, personal communication). The sequential dose-fractionation scheme was 50 Gy/15 fx, 45 Gy/10 fx, and 42.5 Gy/5 fx, and the results have not been reported yet. In our institution, patients with T1 or T2 single vocal cord tumors, without anterior commissural involvement, have undergone boost irradiation with the 3D conformal technique since January 2011. The dose-fractionation scheme involves initial treatment of the larynx (50 Gy/20 fx), followed by boost irradiation of the unilateral vocal cord site (20 Gy/8 fx), with a total of 70 Gy administered to the primary lesion. Between January 2011 and December 2012, a total of 20 patients underwent definitive RT with the boost technique. With short-term follow-up, the local tumor control of the new method was not found to be inferior to the conventional method. In addition, there was no grade 2 or greater chronic laryngitis or edema. Most inflammatory changes of the glottis were mild and asymptomatic, and no further aggravation of the gross findings was observed. Fifteen patients had residual inflammatory signs on the laryngoscopic examinations at 6 months to 1 year after the completion of RT, of whom eight patients showed the ipsilateral hyperemia and wall thickening with the contralateral vocal cord relatively clear and well-healed. Although the boost irradiation technique also treated the whole larynx, the dose reduction in the contralateral side with conformal RT technique showed favorable toxicity profiles. Further studies are required to evaluate the clinical benefit of the single vocal cord irradiation in early glottic cancer.
Conclusion
From the present long-term analyses of definitive RT in early glottic cancer, a high cure rate, tolerable toxicity, and favorable voice quality were obtained. T2 stage and anterior commissural involvement were the most important prognostic factors related to worse local control, and further investigations of the optimal treatment strategies in the high-risk tumors are needed. Although a larger fraction size and shorter overall treatment time showed a potential relationship with better tumor control, longer follow-up is needed to confirm this finding. The higher incidence of ipsilateral local failure points out the importance of reducing recurrences at the site of the primary tumor. In the local field RT of T1-2N0 squamous cell carcinoma of the glottis, optimization of the RT method would be a remaining subject to improve the therapeutic index.
Notes
Conflict of interest relevant to this article was not reported.
Acknowledgements
This work was supported by a grant from the Korea Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (No. A120313), the National R&D program of the Dongnam Institute of Radiological & Medical Sciences funded by the Ministry of Education, Science and Technology (No. 50595-2014), the Interdisciplinary Research Initiatives Program of the College of Engineering and College of Medicine, Seoul National University (2013), and the National Research Foundation of Korea (NRF) funded by the Korea government (No. 2014M2A2A7055063).