The Economic Burden of Breast Cancer in Korea from 2007-2010
Article information
Abstract
Purpose
This study estimates the socioeconomic cost and burden for breast cancer patients in Korea between 2007 and 2010.
Materials and Methods
This study used a prevalence-based approach to estimate the cost of breast cancer. Breast cancer patients were defined as those who were hospitalized or have visited an outpatient clinic during the period from 2007 to 2010. The socioeconomic costs of breast cancer were subdivided into two costs: direct and indirect.
Results
From 2007 to 2010, the prevalence of treated breast cancer increased from 7.9% to 20.4%. The total socioeconomic costs incurred by breast cancer increased by approximately 40.7% from US $668.49 million in 2007 to US $940.75 million in 2010. The direct medical care costs for 2010 were 1.4 times greater (US $399.22 million) than for 2007 (US $278.71 million). The direct non-medical costs rose from US $50.69 million in 2007 to US $75.83 million in 2010, a 49.6% increase. Regarding the economic burden of breast cancer, the total indirect costs were US $339.09 million in 2007 and increased by 37.3% to US $465.70 million in 2010. In the sensitivity analysis, with the annual discount rate for each year ranging from 0%-5%, the costs increased 1.1-1.2 times.
Conclusion
Due to the growing incidence of breast cancer, the annual prevalence and related costs are increasing. We must strive to reduce the socioeconomic burden of breast cancer through preventive measures and early screening.
Introduction
Breast cancer is the second leading cause of cancer mortality among women, behind lung cancer. Moreover, it is the most commonly diagnosed cancer after non-melanoma skin cancer. According to the American Cancer Society, approximately 1.3 million women worldwide are diagnosed with breast cancer annually, and more than 465,000 die from the disease [1].
In Korea, breast cancer had the second highest incidence rate of any cancer at 38.3 per 100,000 people in 2009. In other developed nations, the rates were markedly higher, at 42.7 per 100,000 in Japan, 76.0 in the United States, and 89.1 in the United Kingdom [2]. Moreover, Organization for Economic Cooperation and Development (OECD) countries have reported that breast cancer is the most common cancer in women, followed by colorectal and lung cancer [3]. In addition, the incidence of breast cancer has been increasing by 8.7% annually for the last 10 years, behind thyroid and colorectal cancer [2]. Nevertheless, breast cancer has the highest survival rate compared to other types of cancer; the 5-year survival rate is 33.9% worldwide [3], which is greater than 89% in the United States, 82% in Canada, 85% in Japan, and greater than 90% in Korea, and these rates are gradually increasing [2,4].
Breast cancer is a prominent disease in terms of economics, and the top three cancers that have the greatest economic impact globally are lung cancer (US $188 billion), colorectal cancer (US $99 billion), and breast cancer (US $88 billion) [5].
In 2011, the cost of cancer in Korea accounted for 15%-20% of the total medical costs and 1% of the total health insurance budget [6]. Moreover, cancer treatment costs accounted for 10% of all treatment costs, becoming a burden on national health expenditures [6]. Cancer-related costs in Korea increased 3.9-fold from 119.2 billion won in 2007 to 394.71 billion won in 2011. Costs are expected to rise as society ages and with the development of new technology and other factors [6-8].
Based on estimations of the total medical costs of cancer, including those for patients and survivors, the average patient diagnosed with breast cancer spends 15.95 million won, and patients with other types of cancer with higher survival periods and recovery rates spends even more [9]. Economic burden is often defined as a ‘loss of economic resources and opportunities due to disease’ and it has come to the fore as a prominent aspect of cancer and cancer survival [7]. Estimating the burden of a disease is essential for public health researchers and policymakers. The disease burden estimation evaluates the distribution of medical services, which is used to explain the general status of a population’s health in comparison to the performance of the health system and establish a goal for public health [8,10]. It also evaluates the potential costs and benefits of resources and public health interventions across health research and disease categories [11].
No study has estimated the socioeconomic costs of breast cancer in South Korea, although two studies have examined the socioeconomic costs of major cancers [12,13]. Considering the recent rise in the incidence of breast cancer and associated medical costs, a study of socioeconomic costs change in breast cancer is necessary. This study utilizes the data from health insurance claims to calculate the scale of socioeconomic costs incurred by breast cancer patients between 2007 and 2010 to understand the extent and details of its negative impact. Our goal is to provide the latest data on costs related to breast cancer to understand the increasing cost trends in South Korea.
Materials and Methods
We estimated the cost of breast cancer using a prevalence-based approach. Both preexisting breast cancer patients and newly diagnosed patients between 2007 and 2010 were used to calculate the costs of using medical services to treat breast cancer in South Korea.
We examined the Korea National Health Insurance (KNHI) Claims Database of the Health Insurance Review and Assessment Service (HIRA). In South Korea, the KNHI provides mandatory universal health insurance and covers comprehensive medical care and medical aid. In the KNHI system, health care providers are required to submit claims documenting the provided medical services and prescriptions. This study was authorized by the Deliberation Committee on the Provision of Medical Treatment Information Data of HIRA.
We also obtained 2007-2010 mortality data from the Korean National Statistical Office. All costs were measured using an exchange rate of 1,176 Korean won to US $1 (2010 exchange rate).
The study subjects were breast cancer patients who filed health insurance claims from 2007 to 2010 and had breast cancer (International Classification of Disease 10th ver.; ICD-10 code: C50) listed as a primary diagnosis.
We calculated the socioeconomic costs of the disease by dividing it into direct and indirect costs, based on a previous study [14]. Direct costs are associated with expenses incurred in disease treatment, which consist of direct medical and non-medical care costs. Direct medical costs include outpatient and inpatient care costs paid by the insurer and non-covered care costs paid by patients, such as food expenses, differences in costs due to the use of private wards, fees for special diagnosis, and prescribed pharmaceutical costs. Direct non-medical care costs consist of transportation costs from inpatient and outpatient services and guardian costs. Indirect costs were broken down into lost productivity, opportunity costs incurred due to the time spent at outpatient visits, and hospitalization (Fig. 1).
We used claims data from the National Health Insurance Center (NHIC) and used the costs of claims with C50 as a primary diagnosis from 2007 to 2010 on a yearly basis as the annual medical costs to assess the outpatient and inpatient direct medical costs. However, this does not reflect the costs related to non-covered services, as data from the NHIC include only the costs for medical services covered by the insurance. The non-covered medical costs were estimated based on the survey results of patients of medical care costs; according to this survey, the proportion of non-covered service costs paid by inpatients was 23.8% in 2007, 23.6% in 2008, 43.1% in 2009, and 23.1% in 2010; the proportion of non-covered service costs paid by outpatients was 24.3%, 24.4%, 16.3%, and 18.3% in 2007 to 2010, respectively.
The values were calculated as follows:
Non-covered service costs related to inpatient treatment= (Covered costs for inpatient treatment×The proportion of non-covered service costs paid by inpatients)/(1–The proportion of non-covered service costs paid by inpatients), Non-covered service costs for outpatient visits=(Covered costs for outpatient treatment×The proportion of non-covered service costs paid by outpatients)/(1–The proportion of non-covered service costs paid by outpatients).
To determine the prescription costs, there were no data on the proportion of non-covered pharmaceutical costs. Because most prescribed pharmaceuticals are covered by insurance in Korea, we assumed that non-covered pharmaceutical costs were not incurred to prevent overestimation. Therefore, we used HIRA drug claim records to determine the outpatient pharmaceutical costs.
As for direct non-medical care costs, the annual transportation costs for breast cancer treatment were calculated by summing the products of the average roundtrip transportation costs and the total numbers of outpatient visits, emergency room visits, and hospitalizations in accordance with age. The average roundtrip transportation cost per hospital visit was estimated based on the data from the Korean Health Panel in 2010. The average one-way transportation cost per inpatient visit for a patient and a caregiver was US $6.83. According to the calculation, the cost of a one-way transportation per outpatient visit was US $0.70 [15].
Caregiver costs were calculated by multiplying the average daily caregiver cost of US $48.3 (2005) provided by the Korea Helper Society with the number of hospital stay (day). Then the product was adjusted by a price index to be applicable to a period of 2007-2010, and calculated by taking in account the annual increase in the price index since 2005.
In the case of outpatient visits, it was assumed that patients of age of 0-9 years and 60 years and above would accompany a guardian; thus, multiplied the average daily income in 2005 by the total number of outpatient visits, which then reflected the price index for 2007-2010. Furthermore, the number of hours spent for per outpatient visit was estimated as 1/3 of the working hours, so it was multiplied to the number of outpatient visits.
Indirect costs, characterized as the opportunity costs incurred following the use of medical services or premature death, were determined by calculating the total productivity loss based on the human capital approach. The productivity loss per inpatient was estimated by computing the average monthly working hours and wage as laid out in a report on labor conditions in 2007. Because patients younger than 19 years and older than 70 years were not considered to be of working age, only the productivity losses for patients between the ages of 20 and 69 years were considered. To estimate the average monthly work losses due to outpatient visits, the average visit duration was multiplied by the number of outpatient visits.
Premature mortality costs were defined as the loss of future potential earnings of a person until the age of 69 years as a result of premature death, and were estimated by multiplying the number of breast cancer-related deaths in the period between 2007 and 2010 by the age- and gender-specific average annual income and employment rates for each deceased person [16].
To convert the potential incomes of the age groups into present values, an annual discount rate of 5% was applied. For the sensitivity analysis, the costs of premature death were recalculated using discount rates of 0% and 3% annually.
Results
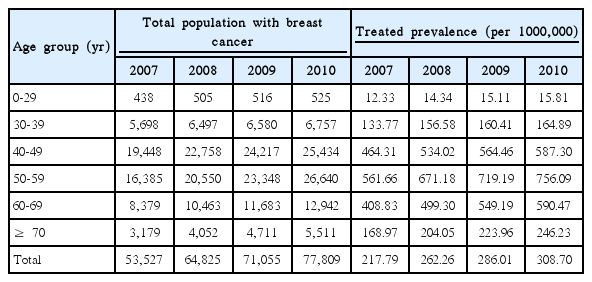
In 2007, there were 53,527 breast cancer patients in South Korea. By age group, the treated prevalence was the highest among women in their 50s at 561.66 per 100,000 people, followed by women in their 40s and 60s. In 2007, the prevalence of treated breast cancer was 217.79 per 100,000 people, which increased by 308.70 in 2010, a 41.7% increase over a 4-year period. In terms of age, the treated prevalence among women 60-69 years of age rose 0.18% from 2007 to 2010, which was higher than the rate among women in their 30s (0.03%) or 40s (0.12%) (Table 1).
In 2007, women in their 40s had a largest share of the economic burden of breast cancer, followed by women in their 50s, 30s, and 60s. The same trend was observed in 2008, 2009, and 2010 (Table 2).
The economic burden of breast cancer was US $668.49 million in 2007 and increased annually until 2010, i.e., US $773.98 million in 2008, US $777.22 million in 2009, and US $940.75 million in 2010, which was 1.4 times greater than the cost incurred in 2007. Specifically, the increase in cost for 2010 was significantly higher than in 2009 (Table 2).
The direct medical care costs in 2007 were US $278.71 million, making up 41.7% of the total costs. The share of costs paid by the insurer was the largest at US $166.13 million. The direct medical care costs in 2008 were 1.4 times higher than in 2007, and the total direct costs in 2010 were 1.4 times higher than in 2007. The total direct non-medical care costs in 2007 were US $50.69 million, composed of transportation costs of US $4.77 million and caregiver costs of US $45.92 million. In 2010, the direct non-medical care costs amounted to US $75.83 million, a 1.5 times increase over 2007. In 2007, the indirect costs were US $339.09 million and accounted for 50.7% of all costs. The lost productivity costs were US $47.28 million, and the costs of premature death were US $291.81 million. The indirect costs of breast cancer in 2010 increased by 1.4 times over those in 2007 (Table 3).
In the sensitivity analysis, the costs of premature death were estimated with discount rates of 5% (current standard discount rate), 3%, and 0%. In 2007, the costs of premature death were US $291.81-451.80 million, and total costs were US $668.49-828.48 million. The total costs were US $773.98-1002.13 million in 2008, US $777.22-996.69 million in 2009, and US $940.75-1,178.61 million in 2010. When a discount rate of 0% to 5% was applied, the average costs increased by 1.3 times (Table 4).
Discussion
We used utilized claims data from the HIRA and Statistics Korea data on the cause of death between 2007 and 2010 to estimate the annual prevalence of treated breast cancer and its economic costs, including both already and newly diagnosed patients. During the 4-year period studied, the prevalence and costs of breast cancer increased gradually. While the prevalence rose by 1.1 to 1.2 times since 2007, the economic costs increased by 1.0 to 1.2 times.
The number of cancer patients who visited medical institutions for cancer treatment was 53,527, 64,825, 71,055, and 77,809 in 2007, 2008, 2009 and 2010, respectively, for an annual growth of 9.5%-21.1%. In a previous study, the number of breast cancer patients increased 59.3% over 5 years to 31,729 [12], and then declined 2% over 2 years to 54,746 in 2005 [13]. A decrease in the number of patients was observed because the data for cancer patients in 2005 were obtained from the Korea Central Cancer Registry, while this study used the data from HIRA. This suggests that there was a discrepancy in how patients were defined. However, considering the increase in the numbers of breast cancer patients between 2007 and 2010, and the rising economic costs of breast cancer from US $668.49 million in 2007 to US $940.75 million in 2010, the economic costs of breast cancer are expected to continue to increase.
The total estimated annual economic costs of breast cancer were US $478 million or 0.08% of the gross domestic product (GDP) in 2002, US $806 million and 0.10% of the GDP in 2005, and 0.06%, 0.08%, 0.09%, and 0.09% of the GDP in 2007 to 2010, respectively. An increase in the economic burden due to cancer is evident [12,13]. In the United States, the estimated cost of breast cancer in 2010 was US $16.5 billion, three times the cost in Korea, and it is expected to increase 1.24 times to US $20.5 billion by 2020. In Korea, the cost of breast cancer increased 1.97 times over a 8-year period, from 2002 to 2010, underlining a more drastic rate of increase in Korea [17].
The total economic cost of breast cancer in Korea was US $668.49 million in 2007, a US $190.49 million increase since 2002. The cost in 2007 decreased by US $137.5 million compared to 2005. In 2010, it increased by US $163.5 million from 2009 [12,13].
The number of patients younger than 40 years was low, while that for patients over 50 years was high; a similar trend is observed in the United States where the prevalence of treated breast cancer increases with age. The economic costs of breast cancer in 2010 increased by 4.8%-5.1% compared to 2007 for women in their 50s and 60s, while the costs declined 4.8% for women in their 40s. This trend concurs with an epidemiological survey [18] in which the distribution of prevalence by age was thought to be influenced by the elderly population, who had less exposure to a Westernized diet. As the diet gradually became Westernized, the economic costs tended to be higher among older age groups. Nevertheless, the treated prevalence was higher among women in their 50s, but the costs remained greater among women in their 40s. Unlike other cancer types, breast cancer is more common among relatively young age groups [19]; hence, health education and pre-screening are necessary for younger women to counter this trend. In this study, the proportion of direct medical care costs declined steadily after 2007, while the proportions of direct non-medical care costs and indirect medical costs increased.
The direct medical care costs in 2002 were US $110 million and these subsequently increased by 1.4 times to US $149 million in 2005. In 2007, the estimated costs were US $278.71 million, double the costs in 2002, and estimated to be US $313.73 million in 2008, an increase of 2.9 times from 2002. In 2009 and 2010, the costs were US $335.2 and US $399.2 million, respectively, representing increases of 3.0 and 3.6 times since 2002. These figures demonstrate a rapid increase in the direct medical care costs since 2007. Compared to 2002, the number of patients grew by 1.7 times in 2005, 1.7 times in 2007, 2.0 times in 2008, 2.2 times in 2009, and 2.5 times in 2010, and the incidence increased 1.07 times [2]. A drastic increase in the direct medical costs, compared to the incidence and treated prevalence, might be due to changes in cancer treatment practices. The ‘Medical cost alleviation policy for critical patients,’ implemented on September 1, 2005, required some non-covered costs to be paid by the insurer and reduced legal user-liable expenditures. On December 1, 2009, out-of-pocket payments for costs incurred by hospitalization and outpatient visits were lowered (from 10% to 5%), and breast cancer treatment benefits were expanded in October 2010 [20].
Direct non-medical care costs were estimated to be 1.22 to 1.99 times higher in 2002 and 2005, at US $62 and US $101 million, respectively, compared to US $50.69 million in 2007. Indirect costs in 2005 were US $556 million, approximately 1.19 times higher than the costs of US $465.7 million in 2010.
Our method differed from that of previous studies [9,12]. The estimated economic burden incurred by cancer in 2005 included males and excluded pharmaceutical costs from outpatient prescriptions in calculating direct medical care costs. Other studies included the use of supplementary alternative therapies in direct costs, assumed that a family member would accompany a patient when estimating transportation costs, and considered the productivity loss of caregivers and guardians in the overall cost estimation [12,13].
The total economic cost of breast cancer in California in 2011 was US $1.43 billion, and 80% of this cost was the value of lost productivity, which resulted from the premature deaths of a large number of young or middle-aged women [21]. In Korea, indirect costs represented the largest share of the total economic costs at 49.5%-51.7%, but this is still lower than in the United States. Due to increased productivity and the breast cancer survival rate, the increase in indirect costs is expected to become smaller [21].
With regard to degree of contribution from each variable to the total cost of breast cancer, indirect costs made the greatest contribution in 2007, at 50.7%. Direct medical care costs made up 41.7% of the total in 2007 and 42.4% in 2010, and direct non-medical care costs increased from 7.6% in 2007 to 8.1% in 2010. Moreover, the total cost of breast cancer relative to GDP increased 0.03% between 2007 and 2010. A rise in breast cancer costs is inevitable due to the increase in factors such as the cancer incidence rate, aging society, cancer survival rate, and incidence of secondary cancer. Therefore, appropriate measures must be taken in response.
Furthermore, breast cancer screening might detect cancer at an early stage and allow early treatment with relatively strong effects at low costs [20,22]. Therefore, cancer screening appears to be essential. The breast cancer screening rate in the United States, where cancer screening studies are being conducted continually, was 70.0% in 2005 [20], which was close to the United Kingdom with 76.9% in 2010 [23]; both significantly higher than Korea with 61.1% in 2010. In the United Kingdom, studies of the breast cancer screening rate and the development of breast cancer risk evaluation programs are in progress [24]. More research on improving cancer screening is necessary in Korea.
There are several limitations to this study. First, the insurance claims data provided by HIRA and the clinical data are inconsistent. Nevertheless, the accuracy of the HIRA disease code can be considered reliable to a certain degree as the National Cancer Registry of Korea and Insurance Claims Data incidence rates gave strikingly similar results. Second, this analysis included only the primary diagnosis from insurance claims data, as incorporating secondary diagnoses might reduce specificity and lead to a discrepancy in medical care costs. However, as this study considered only the primary diagnoses and excluded drug preparation fees, costs might have been underestimated. Third, expenses for variables, such as supplementary products for treatment and improved health, were not determined due to limited data. In previous studies, 84.2% of cancer patients in Korea stated that they had taken biologically based complementary and alternative medicine (CAM) therapies, and 80.2% tried dietary treatments. However, we were unable to estimate the expenses of CAM in this study. Fourth, this study was not able to determine the differentiated direct and indirect costs that consider specifics, such as stage (type), treatment, and breast reconstruction surgery in breast cancer patients. Therefore, a breast cancer study based on a specific approach should be conducted in the future. Finally, intangible costs from a reduced quality of life due to socio-environmental changes, such as psychological pain and instability experienced by patients, as well as their families after diagnosis, were excluded as they were difficult to convert into a monetary value.
Conclusion
In conclusion, we estimated the economic costs of breast cancer in Korea from 2007 to 2010 based on insurance claims data for cancer patients who visited medical institutions nationwide. The economic burden of breast cancer is substantial, which has been increasing gradually over the 4-year study period. To reduce the incidence of cancer, programs related to cancer-associated lifestyle management, early-stage cancer treatment, and cancer survivor management must be expanded and established at the national level to reduce the economic costs incurred from cancer. The results of this study might be used as a baseline data for future policymaking.
Notes
Conflict of interest relevant to this article was not reported.
Acknowledgements
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea. (Grant number HI 13C0729). This study was conducted using data from the Korea National Health Insurance Claims Database of HIRA.