A Phase I/II Trial to Evaluate the Technical Feasibility of Partial Breast Irradiation with Three-Dimensional Conformal Radiation Therapy in Korean Women with Stage I Breast Carcinoma: An Initial Report of the Korean Radiation Therapy Oncology Group (KROG) Study 0804
Article information
Abstract
Purpose
This prospective study was designed to verify the technical feasibility of partial breast irradiation in breast cancer patients with small breasts, which are commonly encountered in Korean women.
Materials and Methods
A total of 40 Gy, administered in 10 fractions on consecutive days (one fraction per day), was prescribed to the isocenters of the fields using three-dimensional conformal radiotherapy (3-DCRT). For all patients, treatment planning and dose parameters strictly adhered to the constraints set forth in the Radiation Therapy Oncology Group (RTOG) 0319 protocol. This study was designed such that if fewer than five of the first 42 evaluable patients received unacceptable scores, the treatment would be considered reproducible.
Results
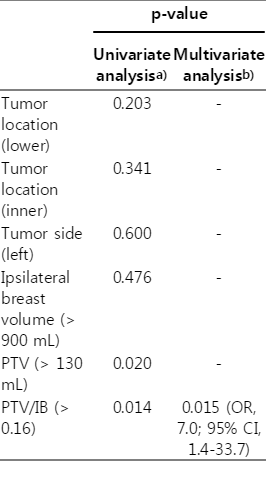
Ten treatment plans (23.8%) were determined to have major variations. There was no major variation in planning target volume (PTV) coverage. The ipsilateral and contralateral breast dose limitations were not met in four (9.5%) and four cases (9.5%), respectively. Major variations in ipsilateral and contralateral lung dose limitations were observed in two cases (4.8%). Major variations in the heart and thyroid dose limitations were observed in one (2.4%) and one case (2.4%), respectively. In multivariate analysis, a ratio of PTV to ipsilateral breast volume (PTV/IB) > 0.16 was the only significant factor that statistically affected major variations.
Conclusion
We concluded that partial breast irradiation using 3-DCRT could not be reproduced in Korean breast cancer patients, particularly small-volumed breast surrogated as PTV/IB > 0.16. The dominant cause was the major variation in surrounding normal breast tissues.
Introduction
A systematic review and meta-analysis of the current randomized trials to evaluate the role of accelerated partial breast irradiation (APBI) in eligible breast cancer patients suggested that APBI did not appear detrimental to survival and could be used as an alternative to whole breast irradiation (WBI) [1-3]. In selected patients, APBI, with fewer larger fractions delivered over a shorter time, could be an alternative to WBI because most relapses occur near the lumpectomy site [4-6].
The high “elsewhere” failure throughout the review of APBI frontier studies indicated the importance of appropriate patient selection and optimal APBI techniques [7]. A phase II study of APBI using proton therapy conducted in Korea showed excellent disease control [8]. However, only one center in Korea is equipped with proton therapy. Therefore, we adopted the three-dimensional conformal external beam radiotherapy (3-DCRT) technique for partial breast irradiation (PBI) because it is noninvasive, compared with brachytherapy or intraoperative therapy, and readily available in many institutions. The Radiation Therapy Oncology Group (RTOG) 0319 study reported that the technical feasibility of 3-DCRT for APBI was acceptable [9,10]. However, the 3-DCRT approach treats comparatively large normal breast tissue volumes while delivering relatively homogeneous doses to the target volume, as the basic underlying principle for the successful application of PBI is balanced radiation delivery between the planning target volume (PTV) and normal breast tissue.
We need to determine whether the technical feasibility confirmed in Western breast cancer patients could be equally applicable to Korean women, who have relatively small breasts compared to Western women. Therefore, we designed phase I and II clinical trials to evaluate the technical feasibility of 3-DCRT in Korean breast cancer patients, using the technique confirmed by RTOG 0319, to determine the types of variations that occur during PBI with 3-DCRT in small-volumed breast cancer patients. This is the first report of the technical feasibility of PBI with 3-DCRT in Korea.
Materials and Methods
1. Patient eligibility
We defined the inclusion criteria more strictly than that of RTOG 0319; the criteria were postmenopausal women, a unifocal tumor, tumor size ≤ 2 cm with a resection margin (RM) > 2 mm, negative sentinel or axillary nodes, hormone receptor positivity, and a good to excellent postoperative cosmesis score [11]. Patients with histological evidence of lymphovascular invasion, an extensive intraductal component, lobular histological type, ductal carcinoma in situ or lobular carcinoma in situ, and wound issues were excluded. Patients who received chemotherapy were also excluded. Radiation must have been initiated within eight weeks after surgery. The institutional review board approved this phase I/II trial, and all patients were prospectively enrolled and submitted consent forms.
2. Treatment techniques and imaging
Patients were immobilized in the supine position with both arms elevated upward, using a vacuum immobilization device. The ipsilateral whole breast and breast surgical scar were marked with a radiopaque rubber catheter. A treatment planning computed tomography (CT) scan (Hi-Speed FX/I, GE Medical Systems, Milwaukee, WI) was performed at a 3-mm scan width, and a contrast-enhanced image was obtained. The scan began at or above the mandible to beyond the breast tissue, including the entire lung. We used the Varian Eclipse treatment planning system (Varian Medical Systems, Palo Alto, CA). The following structures were contoured manually by the radiation oncologist: the lumpectomy cavity (LC) volume, PTV, ipsilateral breast, contralateral breast, thyroid, ipsilateral and contralateral lungs, and heart. We defined the target volume from the LC. To reduce the variability in LC contouring, radiation oncologists who participated in this study were educated and accustomed to the target volume definition guidelines. We assigned a clarity visualization score (CVS) to each patient, as follows; CVS-1, no cavity visualized; CVS-2, cavity visualized but significant uncertain margins; CVS-3, cavity visualized with some uncertain margins; CVS-4, cavity with mild heterogeneity on CT and mostly distinct margins; CVS-5, homogenous cavity with clearly identified margins [12]. The PTV was nonuniformly expanded 5-15 mm around the LC, depending on the safety margin widths along the six directions (superior, inferior, medial, lateral, superficial, and deep) described in the surgical pathologic report. We set a 1.5 cm expansion if the RM was < 1 cm, a 1-cm expansion if the RM was between ≥ 1 cm and < 2 cm, and a 0.5 cm expansion if the RM was ≥ 2 cm in all six directions. The PTV excluded the skin, was confined to a maximum of 5 mm under the skin, and vexcluded the underlying lung by lung-chest wall interface. Ipsilateral and contralateral breast included all tissue volume, excluding pectoralis muscles, chest wall muscles, and ribs as recommended by RTOG.
The treatment was administered with three-dimensional conformal fields, and intensity-modulated radiation therapy was not allowed. Three or four non-coplanar beams that used 6-MV photons or a mixed-modality plan that used a photon field with an en face electron field were used. The maximum dose should not exceed 110% of the prescribed dose. We followed the radiotheraphy delivery technique and dosimetric guidelines for dose volume constraints set forth by the RTOG 0319 study. A thorough review of the dose volume histogram of each patient was performed by both the radiation oncologist and physicist, and a quality assurance evaluation of the treatment plans was performed to determine the variations.
Each plan was scored as acceptable (per protocol), marginally acceptable (minor variation), or unacceptable (major variation). An acceptable plan showed 95% isodose surface covers 100% of the PTV, and all specified critical normal tissue dose limits have been met. A marginally acceptable plan showed 95% isodose surface covers between ≥ 95% to < 100% of the PTV, and all specified critical normal tissue dose limits fall within 5%. An unacceptable plan showed 95% isodose surface covers < 95% of the PTV, or any critical normal tissue dose limit exceeding 5% of the specified value. Each dose limitation for normal tissues followed the criteria described in the RTOG 0319 protocol [9].
In brief, less than 50% of the ipsilateral whole breast should receive ≥ 50% of the prescribed dose and less than 25% of the whole breast should receive the prescribed dose. The contralateral breast should receive less than 3% of the prescribed dose to any point. At most, less than 10% of the ipsilateral lung can receive 30% of the prescribed dose and less than 10% of the contralateral lung should receive 5% of the prescribed dose. In right-sided lesions, less than 5% of the heart should receive 5% of the prescribed dose in a while the volume of the heart receiving 5% of the prescribed dose should be less than that for treatment using conventional whole breast radiation with tangential fields in left-sided lesions. Maximum point dose in thyroid should be less than 3% of the prescribed dose.
A total of 40 Gy, given in 10 fractions on consecutive days, one fraction per day, were prescribed to the isocenters of the fields. Electronic portal imaging was monitored for the first session and repeated at the sixth radiotherapy session. No patients received chemotherapy, and adjuvant endocrine therapy was combined with radiotherapy in all patients.
3. Statistical considerations
Technical feasibility was the primary end point in this study. A final review of the plan as acceptable or marginally acceptable indicated that the technique is reproducible. An optimal two-stage Simon design was used for this trial. Let p-value be the true probability that the final review is acceptable or marginally acceptable. A p-value close to 1 implies that the radiation therapy is reproducible in a multi-center setting. If p-value is ≤ 80%, the goal is to have at most a 5% probability of concluding that the technique is reproducible. On the other hand, if p-value is ≥ 95%, the desired level, the goal is to have at most a 10% probability (five cases) of concluding that the technique is not reproducible in the first 42 evaluable treatment plans. Associations with pretreatment factors, including the tumor location, tumor side, ipsilateral breast volume, PTV volume, and PTV volume to ipsilateral breast volume ratio (PTV/IB) were tested using the chi-square test and logistic regression. Fisher’s exact test was used with small sample sizes (< 5 in any cells) in univariate analysis. All statistical data were processed using SPSS ver. 19.0 (SPSS Inc., Chicago, IL), and null hypotheses were rejected at p < 0.05.
Results
1. Patient characteristics
A total of 42 patients were enrolled in this study between January 2009 and July 2013. The pretreatment characteristics are shown in Table 1. The median age of patients was 62 years, and the median tumor size was 11 mm. The tumor location was the outer or central quadrant for 37 patients (88%) and the inner quadrant for five patients (12%). The median LC volume at the time of treatment planning was 34.88 mL. The median PTV volume was 108.94 mL. The median ipsilateral whole breast volume was 784.18 mL. The median PTV/IB ratio was 0.1481 (Table 1).
2. Technical feasibility
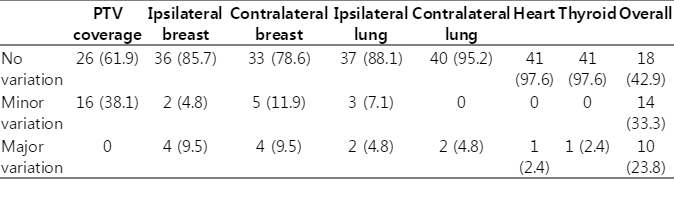
Results of the plan evaluation with regard to dosimetric variations for the 42 patients, upon which the decision of feasibility was based, are shown in Table 2. There were no variations in 18 patients (42.9%) and minor variations in 14 patients (33.3%). Ten treatment plans (23.8%) were determined to have major variations, all of which were related to normal tissue dose constraints that exceeded 5% of the specified limit. There were no major variations in the PTV coverage. Figs. 1 and 2 show dose distribution and dose volume histogram of a case determined to have no major variation.
Technical feasibility of radiation treatment planning using three-dimensional conformal radiotherapy
Dose distribution of partial breast irradiation using two coplanar and two non-coplanar photon beams.

Dose volume histogram of partial breast irradiation using two coplanar and two non-coplanar photon beams. Lumpectomy cavity (purple), planning target volume (red), ipsilateral breast (yellow), contralateral breast (cyan), ipsilateral lung (blue), contralateral lung (green), and heart (orange) are depicted.
We analyzed the relationship between the tumor or normal tissue parameters and major variations in the treatment plans (Table 3). Of 12 patients with PTV > 130 mL, six (50%) had major variations. However, only four of 30 patients (13.3%) with PTV ≤ 130 mL had major variations. Major variations were observed more frequently in patients with PTV/IB > 0.16 (seven of 15 patients, 46.7%) than in patients with PTV/IB ≤ 0.16 (three of 27 patients, 11.1%). In multivariate analysis, the PTV/IB showed statistical significance affecting the major variation.
3. Dosimetric features in cases with major variations
Dose limitations in the ipsilateral and contralateral breast were not met in four (9.5%) and four cases (9.5%), respectively. Case no. 13 had major variations in both ipsilateral and contralateral breast dose limitations (Table 4). In this case, PTV was more than 130 mL (148.16 mL) and PTV/IB was more than 0.16 (0.19). In the four cases with major ipsilateral breast variations, all had PTV/IB > 0.16, and three cases had PTV > 130 mL. Six cases with PTV > 130 mL (case nos. 9, 13, 18, 27, 28, and 42) and seven with PTV/IB > 0.16 (case nos. 13, 18, 23, 27, 28, 31, and 42) had major variations. Among these cases, four with PTV > 130 mL (66.7%) and five with PTV/IB ratios > 0.16 (71.4%) did not fit the ipsilateral or contralateral breast dose limitations.

Dosimetric features in cases with major variations of treatment planning using three-dimensional conformal radiotherapy
In the analysis of ipsilateral lung dose constraints, two cases (4.8%) showed major variations. Ipsilateral breast volumes < 900 mL and PTV/IB ratios > 0.16 were observed in both cases. In two cases with major variations in the contralateral lung dose limitation, we did not observe any specific features. Only one case (2.4%) had a major variation in the heart. In this case, the tumor was located in the lower central portion of the right breast. Although an electron beam was used in part in this case, more than 2 Gy were delivered to the right atrium. A thyroid dose limitation was observed in one case (2.4%). In this case, the LC was in the upper quadrant of the left breast, near the thyroid gland (Table 4).
Discussion
As clinical experiences with PBI increase, it is certain that patient subsets might be adequately treated with PBI, with acceptably low recurrence rates. As PBI currently remains an investigational approach and is not yet a standard therapy, we designed this study to include a more rigorously selected group of patients than would be allowed by the “suitable” criteria suggested in the American Society for Radiation Oncology consensus statement [2]. We further limited eligible patients for this study to those without wound issues and chemotherapy and those with good to excellent cosmesis scores at the time of radiotherapy.
Delineation of the optimal treatment volume required to obtain equal or better local control rates, compared with WBI, after conservative surgery is crucial to the precision of conformal radiation therapy planning and the validity of clinical trial results [13]. The issue of surgical clips during LC visualization when performing PBI with 3-DCRT has been highlighted as mandatory [14]. However, surgeons at our institute do not use surgical clips; therefore, we used the LC to define the PBI treatment target. In a study of change of the serial morphologic cavity after surgery, the optimal time to delineate the target volume from the excision cavity in the planning CT scan for PBI was reported to be within eight weeks [15]. Based on this data, we limited study entry to patients who could undergo PBI within eight weeks after surgery. Variability among radiation oncologists regarding delineation of the postsurgical LC could be decreased with a CVS ≥ 3 [12]. In our study, CVS < 3 was observed in only one patient. For this patient, when defining the LC, we obtained a consensus among radiation oncologists to include all surgical tissue extensions. We chose a different method to define the PTV than that used in the RTOG 0319 study. We differentiated the optimal margin to be included in the PTV according to the surgical safety margin. This was meant to provide the same final margin to the gross tumor area in all patients, irrespective of the extent of volume surrounding the gross tumor that was surgically removed.
The widespread acceptance of APBI using the 3-DCRT approach is likely because it is totally noninvasive and delivers a homogenous dose distribution to the target volume. In our study, PTV was defined to exclude the skin (5 mm beneath the skin surface) in order to reduce skin toxicity [16] and there was no case in which skin should be included in PTV due to positive or close superficial RM. And, there was no major variation in the PTV coverage because the beam-aperture was composed to cover the PTV. The majority of the major variation was caused by the inability to fit the dose constraints on normal breast tissue. The surrounding normal tissue dose-volume relationship is a critical underlying factor, in accordance with the dosimetric guidelines. Regarding the PTV/IB ratio, large target volumes (PTV) contribute to an increased risk of severe fibrosis and poor cosmesis [17]. Leonard et al. [18] reported a clear and statistically significant association between the dose-volume parameters and late moderate-to-severe breast toxicity. The relative volumes of breast tissue that receive low and high percentages (V5%-V100%) of the prescribed dose were associated with the risk of subcutaneous fibrosis, and the volume receiving 50%, 80%, and 100% (V50%-V100%) of the prescribed dose was associated with fair/poor cosmesis scores. These results generally demonstrate a higher incidence of late normal tissue toxicity compared with those reported in the RTOG trials with 3-DCRT APBI [9,10]. In order to substantially reduce the risk of adverse normal tissue effects, the authors suggested the use of more restrictive dose-volume constraints than those currently defined by the National Surgical Adjuvant Breast and Bowel Project (NSABP) B39/RTOG 0419 trial. However, the authors noted a potential limitation of the retrospective analysis in that a baseline postsurgical evaluation was not performed, thus making it difficult to assess the true adverse effects of radiation-induced normal tissue toxicity; therefore, additional results are needed before these suggestions can be accepted.
In our study, the ipsilateral breast dose limitations of V50% < 50% were not acceptable in four cases (9.5%), while, there was no violation of the ipsilateral breast dose limitation in the RTOG 0319 study [9]. As a possible explanation for the discordance between the two studies, we can consider the differences in breast size. In a recent phase I/II study of APBI with 3-DCRT in Western countries [19], the median ipsilateral breast volume, 1,698 mL (range, 647 to 3,627 mL), was 2-fold larger than that in our study, 784 mL (range, 337 to 1,446 mL). The median V50% of the ipsilateral breast was 41.9% in our study (data was not shown), and this parameter was larger than that reported in Western countries (37.9%). In a Korean study of dosimetric comparison of PBI with four different techniques, mean V50% in 3-DCRT was 57.6%, and this parameter is similar to our data [20], meaning that relatively larger portions of the normal breast tissue might be exposed to low-dose irradiation (V50%) in Korean women with small breasts. In addition, four cases (9.5%) showed major variations in contralateral breast dose limitations. In these cases, only one had an ipsilateral breast dose violation. There was a limitation in the gantry angle of the linear accelerator with regard to fitting the ipsilateral breast dose limitation, and this could cause partial contralateral breast irradiation in small breasts. Comparatively large normal breast tissue could be exposed to low-dose irradiation by use of PBI with 3-DCRT while relatively homogeneous doses could be delivered to the target volume. Therefore, the ipsilateral breast dose limitation in the RTOG 0319 study might not be applicable to Korean women with smallvolumed breasts.
Conclusion
Although we could not draw the same conclusion regarding technical feasibility as in the RTOG 0319 study, we can conclude that the PTV/IB ratio affects the technical feasibility of 3-DCRT planning for PBI and it can be performed in Korean breast cancer patients with PTV/IB ≤ 0.16, even those with small breasts. In addition, further study is needed in order to determine feasible dose limitations, particularly breast limitation, when PBI with external-beam irradiation is administered to small-breasted patients.
Notes
Conflict of interest relevant to this article was not reported.