INTRODUCTION
Peripheral T cell lymphomas (PTCL) include those heterogeneous malignant lymphocytic neoplasms of a post-thymic T-cell phenotype origin. Primary testicular lymphoma is defined as testicular involvement at the time of diagnosis, and this is a rare disease that accounts for about 1% to 8% of all testicular cancer (1). It is more frequent in men older than 60 years of age (2). A considerable relapse rate to extranodal sites, such as the central nervous system or the contralateral testicle, has been reported despite of using doxorubicin-based chemotherapy for treating testicular lymphoma patients (1). Ocular manifestation of a primary T-cell lymphoma of the testis is extremely rare (3). Herein, we report on a case of a testicular PTCL patient with the ciliary body of the eye being the primary site of relapse, and this man died of leptomeningeal seeding.
CASE REPORT
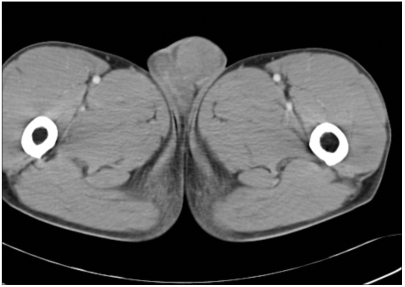
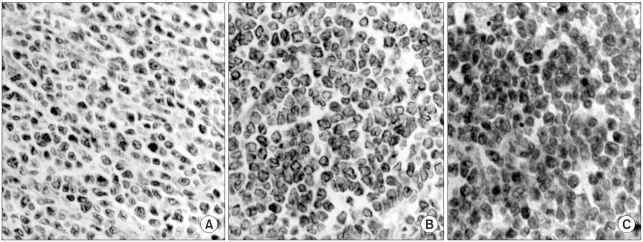
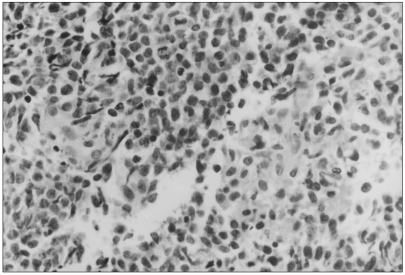
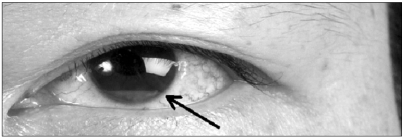
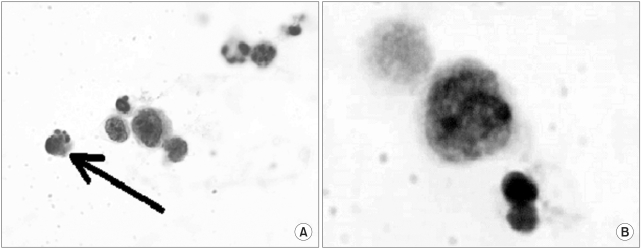
A 43-year-old man presented with a painless testicular mass (Fig. 1). The pathologic diagnosis of the radical orchiectomy specimen revealed PTCL-u (Fig. 2), and further staging evaluation (bone marrow biopsy, computerized scan of the abdomen, pelvis and nasopharynx, and cytology of the cerebrospinal fluid) showed a right nasopharyngeal mass (Fig. 3). which was also confirmed as PTCL-u (Fig. 4). Immunohistochemical staining showed CD3(+), CD4(-), CD20(-), CD56(+), CD68(-), granzyme(-) and Epstein-Barr virus(-). His clinical stage was III according to the Ann Arbor staging system. He received the first-line chemotherapy with four courses of CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) regimen followed by involved-field radiotherapy (4400 cGy) to the testis and nasopharynx, and he subsequently achieved complete remission according to the International Working Group criteria. Two months after achieving complete response, the patient complained of progressively worsening vision in his left eye. The external eye examination was normal except for a pseudohypopyon in his left eye (Fig. 5). The vitreous and posterior segments were normal as were the conjunctiva, lens and sclera of the left eye. The intraocular pressures were 12 mmHg in the right eye and 15 mmHg in the left eye. The ultrasound biomicroscopic imaging of his left eye revealed a mass-like lesion in the left ciliary body, so anterior chamber aspiration was performed. The cells obtained in the aqueous aspirate were described morphologically as atypical lymphocytes with mercury drop-like apoptotic bodies (Fig. 6), which were characteristic of lymphoma. The CSF examination, brain imaging and the abdomen and pelvis computerized scanning showed no evidence of disease recurrence. A week after initiation of chemotherapy with high dose cyclophosphamide, the follow-up ultrasound biomicroscopic imaging showed complete disappearance of the infiltration and the anterior chamber aspirate was cleared. Following autologous peripheral stem cell transplantation, he achieved a second complete remission (International Working Group criteria). Yet three months after the patient achieved his secondary complete remission, the patient developed dysphagia. Esophagogastroduodenoscopy and computerized scanning of the pharynx could not reveal the cause of the dysphagia. A modified barium swallowing test showed ataxia of the pharyngeal wall motion. Magnetic resonance imaging of the brain demonstrated parenchymal enhancement of the cerebellum, linear enhancement at the anterior aspect of both cerebral peduncles and tiny enhancing foci of the left parietal cortex (Fig. 7). Leptomeningeal seeding was confirmed by cytologic examination of the cerebrospinal fluid. Treating him with intrathecal methotrexate was unsuccessful; the patient succumbed to the disease 11 months after the initial diagnosis.
DISCUSSION
PTCLs are a heterogeneous group of neoplasms that present as advanced disease, and they are characterized by widespread dissemination, aggressive behavior and very poor survival. Primary testicular lymphoma accounts for 1% to 2% of all non-Hodgkin's lymphoma and the most common subtype of testicular lymphoma is diffuse high-grade B-cell lymphoma (1). Both B- and T- cell testicular lymphomas have a tendency for extranodal manifestation such as in the skin, Waldeyer's ring, the CNS, bone marrow and in the contralateral testis at the time of presentation or relapse (4). This case is a rare example of an ocular recurrence of a primary T-cell lymphoma of the testis, and only 6 such cases have been reported in the literature (3). Because the eye, the central nervous system and the testis have a distinct anatomical feature, that is, a blood-organ barrier that prevents the free circulation of the lymphoid cells, it has been proposed that neoplastic clones may have a selective advantage of being able to cross blood-organ barriers during the evolution of lymphoma (5). Moller et al. suggested including routine CNS prophylaxis into the treatment of testicular lymphoma (1).
Primary ocular lymphoma involves the vitreous and retina, and often as part of primary CNS lymphoma (3). Secondary ocular lymphoma involves the uvea in systemic disease (3). The typical signs of lymphoma's ocular involvement include anterior uveitis, vitreous opacities, chorioretinitis and flank retinal detachment (3). In this case, the ciliary body involvement followed the manifestation of aggressive systemic T-cell lymphoma.
An aggressive course of primary testicular T-cell lymphoma has been reported by other studies too (2,3,5,6). Despite of aggressive treatment with high-dose chemotherapy and autologous stem cell transplantation as salvage therapy in this patient, the patient experienced a short-term relapse in the leptomeninges. Fonseca et al. reported an 80% recurrence rate of primary testicular lymphoma after systemic chemotherapy and of the recurrent cases, 32% involved the CNS (7). They insisted that intrathecal prophylactic chemotherapy was not effective because most of the case of CNS recurrence involved the brain parenchyma (7). Though the leptomeningeal recurrence pattern seen in our patient was a rare pattern for testicular lymphoma, any methods of CNS prophylaxis such as irradiation or intrathecal chemotherapy should be considered at the moment of discovering ocular involvement. The recurrence patterns of testicular lymphoma should be kept in mind when physicians are determining an effective management strategy for treating patients with primary testicular lymphoma.