Trends of Mammography Use in a National Breast Cancer Screening Program, 2004-2008
Article information
Abstract
Purpose
Korea started breast cancer screening as part of the National Cancer Screening Program (NCSP) in 1999. In order to identify under-served groups, we investigated mammography uptake in the National Breast Cancer Screening Program.
Materials and Methods
The study population was participants in the National Breast Cancer Screening Program from 2004 to 2008. We analyzed participation rates by insurance type, age group, and area of residence.
Results
Total participation rates for breast cancer screening increased from 18.2% in 2004 to 35.0% in 2008. The participation rate in the group aged 60 to 69 years showed the greatest increase, 21.3%, among the four age groups. Although the screening rate increased continuously, the participation rate of the Medical Aid Program (MAP) group was low compared to the National Health Insurance (NHI) group. Moreover, the increasing trend of mammography uptake in the MAP group was much lower than that of the NHI group.
Conclusion
The participation rate for breast cancer screening in the NCSP in Korea has increased. However, the participation rate in mammography among MAP recipients is still lower than that of NHI beneficiaries. To increase mammography uptake, it is important to make it available to everyone by ensuring inclusion of all population subgroups.
Introduction
Breast cancer has been the most common cancer among Korean women and will continue to increase for the next 20 years (1). Mortality rates for breast cancer in Korea have increased from 3.7 per 100,000 in 1993 to 4.6 per 100,000 in 2002 (2).
Breast cancer is one of the leading causes of cancer death in Korea. Although the incidence of female breast cancer is still low in Korea, compared to that of European countries and the United States, its incidence and mortality have been rising rapidly (3). It is expected to increase steadily with the Westernization of lifestyle (e.g., increased fat intake) and exposure to hormone-related risk factors such as early menarche, late menopause, no or late birth and hormone replacement therapy (4).
Cancer screening can be offered to a population using opportunistic or organized models. Organized screening programs have nationally implemented guidelines that define who should be invited, how frequently they should be screened, and how any screening-detected abnormalities should be followed-up and treated. Opportunistic screening depends on individual members of the public requestinsg screening, or on their health advisors recommending screening (5). In Japan, mass screening for breast cancer is performed every 2 years for women over the age of 40 (6). Most European countries have established nationally or regionally organized programs, and almost all include an invitation for mammography every 2 years (7). The American Cancer Society and the National Cancer Institute advise screening every 1-2 years (8).
In 1999, Korea began organized screening for breast cancer as a part of the National Cancer Screening Program (NCSP), which covers Medical Aid recipients. The target population was expanded to include National Health Insurance (NHI) beneficiaries within the lower 20% income bracket from 2002, and the lower 50% since 2005. The NCSP provides screening services free of charge for Medical Aid Program (MAP) enrollees and people who have NHI with premiums below 50%. Breast cancer screening with mammography is recommended every 2 years for women aged ≥40 years old.
Until now, there have been few nationwide studies of mammography uptake in organized programs in Korea. In order to identify under-served groups, we investigated mammography uptake in the National Breast Cancer Screening Program.
Materials and Methods
We used data from the NCSP from 2004 to 2008 and analyzed participation rates by age, insurance, and area. Age was divided into four categories: 40-49, 50-59, 60-69, and ≥70 years old. There were two types of insurance status: MAP and NHI. Area of residence was classified into two groups: metropolitan (Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, and Ulsan) and provincial (Gyeonggi, Gangwon, Chungcheongbuk, Chungcheongnam, Jeollabuk, Jeollanam, Gyeongsangbuk, Gyeongsangnam, and Jeju). Although the NCSP started breast cancer screening since in 1999, the NCSP database was only computerized in 2002 and was stabilized from 2004. Therefore, we analyzed participation rates for breast screening from 2004 to 2008.
Results
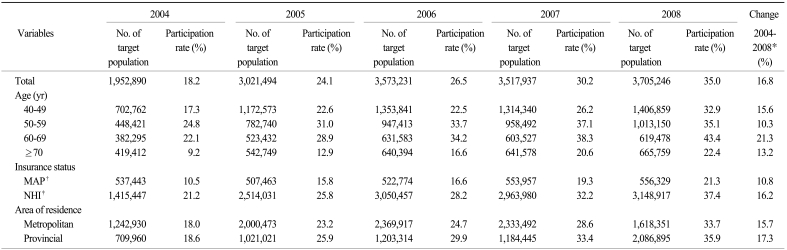
The total target population for breast cancer screening increased from 2004 to 2008, as did participation rates (Table 1). The target population was 1,952,890 in 2004 and 3,705,246 in 2008. The total participation rate increased by 16.8% from 2004 to 2008. Participation in the 60-69 years age group showed the greatest increase, 21.3%, among the four age groups during the period. The ≥70 years age group showed the lowest participation rate during this period. The participation rate in the MAP group was 10.5% in 2004 and 21.3% in 2008. The participation rate in the NHI group was 21.2% in 2004 and 37.4% in 2008. The change in rate in this latter group was 16.2%, which was higher than that in the MAP group. The change in participation rate from 2004 to 2008 was 15.7% for those in metropolitan areas and 17.3% for those in the provinces.
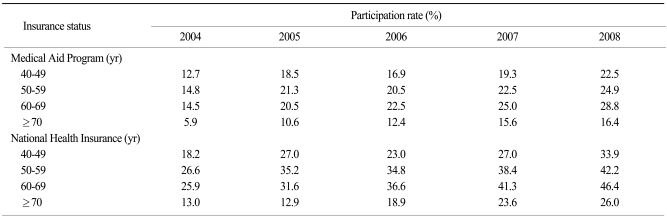
Table 2 shows the trend in participation rates according to age in the MAP group and NHI group. Participation rates increased in all age groups, regardless of insurance type, from 2004 to 2008. The rate among NHI beneficiaries was higher than among MAP recipients during this period for each age group.
Discussion
The size of the target population increased continually from 2004 to 2008, as did participation rates. These findings are encouraging because they represent a steady increase in participation rates overall, the number of people in whom cancer might be prevented, and those who have received early treatment as a result of early detection.
In the present study, the total screening rate for breast cancer screening increased from 18.2% in 2004 to 35.0% in 2008. Although the screening rate increased every year, it is still low compared with that of Western countries: 70.0% in the United States in 2003 (9), and 75.9% in England in 2007 (10). Meanwhile, although Japan started screening in 1987, the participation rate in 2006 was only 12.9% (11) which was low compared with 26.5% in Korea in 2006. Because every country has different eligibility criteria in breast cancer screening due to differences in health care systems, comparison of screening rates between countries needs careful interpretation. For example, the National Health Service Breast Screening Program in United Kingdom provides free breast cancer screening for women aged 50 years or older (12) while the NCSP in Korea provides free screening for women aged 40 years or older for MAP recipients and NHI beneficiaries with premiums below 50%.
Breast cancer screening is increasingly recognized as a crucial tool in the control of cancer, especially given that mammography can decrease breast cancer mortality rates by 20-30% (13). However, unless widely and regularly used, screening cannot be optimally effective in a population (14). Therefore, it has to take place alongside strategic interventions designed to encourage a high participation rate in the eligible population.
In this study, we found MAP enrollees to be an underserved group due to their low socio-economic status. Unfortunately, participation rates for MAP recipients only increased a little during the study period. Previous studies have observed differences among social classes (15,16). Furthermore, it has been shown that screening rates among lower socioeconomic groups are still low, and that morbidity and mortality rates have not been reduced (17). Some previous studies indicate persistent income disparities in cancer screening even when the testing fee is inexpensive or fully reimbursed (5). Practical barriers to screening remain an issue in both organized and opportunistic settings. These practical barriers may include geographic factors, fear of painful procedures, access to health care, demands on time, and underlying health status of the potential participants. Even in organized screening settings, attitudes, beliefs, and knowledge are consistently associated with screening use. Breast cancer screening rates in the United States are low among low-income women and minority women who live in geographically isolated areas (18). These women may be less likely to take advantage of preventive care because of greater demands at home and at work, lack of available transportation, or lack of a regular source of medical care or physician referral (19). To increase the participation rate among lower socioeconomic groups, such as MAP recipients in Korea, it is necessary to continue monitoring the trends and variations in breast cancer screening. It also requires health care support and national awareness, as well as focused management on the part of community health centers. For example, improvement of access to screening services for MAP recipients through the provision of out-of-hours screening services and the increase of facilities in remote areas may enhance breast cancer screening rate for MAP enrollees. To increase participation and reduce disparity in cancer screening, additional individual-directed interventions in cancer-screening implementation are required e.g. individualized in-person or telephone counseling, and individualized letters and reminders, especially for the lower socioeconomic groups (20,21). In the United States, the strongest methods of mammography-promoting interventions have been access-enhancing interventions followed by individual-directed interventions in health settings. Other access-enhancing interventions included mobile vans, help with appointment/scheduling, dependent care, and navigation of the health care system (22). Some European countries are beginning to introduce interventions focused on improving health behavior and increasing access to health care, in order to increase the screening rates among people of lower socioeconomic status (23).
The 40-49 year age group had a low participation rate, as compared with the other age groups, except the ≥70 years age group. There is a need to promote mammography use for women in their 40s because mammography has been shown to reduce breast cancer mortality in women aged ≤40 years in Asia (24).
The present study reveals trends in the participation rates for breast cancer screening at the national level, and for underserved groups according to age or insurance status. It is important to make screening available to everyone by ensuring inclusion of all population subgroups. Intervention is essential to encourage participation and maximize adherence to screening recommendations. In this regard, additional individual-directed interventions in health care settings are required such as in-person or telephone counseling, letters and reminders, or other individual-directed strategies, especially for vulnerable individuals (22). Also, to increase mammography uptake, we recommend that policies emphasize the effectiveness of mammography, and that public health services provide education and information about the service. Outreach campaigns should be designed, through collaboration between community organizations and government health care services, to target specific population subgroups.
Conclusion
The participation rate for breast cancer screening in the NCSP in Korea has increased. However, the participation rate in mammography among MAP recipients is still lower than that of NHI beneficiaries. To increase mammography uptake, it is important to make it available to everyone by ensuring inclusion of all population subgroups.
Notes
This study is supported by a grant from the National Cancer Center (Grant No. 1010200).