AbstractPurposeThe study aimed to assess the differences in dental maturation between childhood cancer survivors and healthy children.
Materials and MethodsFifty-nine cancer patients including 16 (27.1%) girls and 43 (72.8%) boys, aged between 4 and 16 years, underwent dental and radiographic examinations. The mean duration of anticancer therapy was 16.8 months (range, 1 to 47 months), and 4.6 years (range, 8 to 123 months) had passed since the termination of disease. The control group consisted of 177 panoramic radiographs of age- and sex-matched healthy individuals. Dental age (DA) was estimated with Demirjian’s scale and delta age, i.e., DA–chronological age (CA), was used to compare groups.
ResultsThe DA of cancer survivors was accelerated by almost 1 year compared to their CA (9.9±3.1 vs. 8.9±2.8, p=0.040). The greatest difference was observed among patients with brain tumor: delta (DA–CA) was 2.2±1.1 years. Among all cancer patients, only children with familial adenomatous polyposis (FAP)-associated hepatoblastoma (HP) demonstrated delayed DA, with regard to both other cancer survivors (p=0.011) and healthy patients (p=0.037). All four patients with HP suffered from FAP, and three of them had documented adenomatous polyposis coli (APC) genes mutation. The DA of cancer patients having teeth with short roots was significantly greater than that of the cancer survivors without this anomaly (12.8±3.2 vs. 9.0±2.4, p < 0.001).
IntroductionChildren with cancer suffer from various immediate and distant complications of the disease and its long-term therapy. It is known that chemo- or radiotherapy can inhibit the development of almost all organs, and can impair the quality of life of the patient, or even threaten it [1]. Of the dental complications affecting cancer survivors as a result of treatment, the most common are short roots, lack of tooth germs, microdontia, caries, enamel opacity, or gingivitis [2]. It has been found that almost two-thirds of children cured from cancer had at least one dental anomaly [3].
Oncotherapy can directly or indirectly disturb the development of the tooth germ [4]. Both multiple-agent therapy and radiation exposure of more than 20 Gy are significantly associated with an increased risk of more than one dental anomaly [5]. The trials on mice have found that cyclophosphamide, a drug commonly used in cancer therapy, can arrest the process of tooth root elongation by speeding up the closure of their apex [4].
In the first few years of human life, permanent tooth germs hidden in the bone of jaws undergo a process of formation and tissue maturation. This process is very sensitive and regulated by genes, molecules, and signaling pathways [6]. All tooth germs follow the same developmental process, and this can be divided into eight stages based on histology and morphology: A-bud, B-cap, C-bell, D-dentinogenesis, E-amelogenesis, F-appositional dentin and enamel, G-eruption and H-functional. At the age of around six years, the first permanent molar appears in the mouth. It should be stressed, however, that tissue mineralization and root formation do not depend strictly on the terms of eruption. Therefore, to assess the maturity of tooth development in children, it is not sufficient to determine only these factors, and other techniques of assessing dental age (DA) are needed. One of the most common scoring systems is one proposed by Demirjian et al. [7], which is based on the radiological appearance of the seven developing teeth on the left side of mandible: the central and lateral incisors, canines, first and second premolars, first and second molars.
The aim of the study was to evaluate DA of cancer survivors and to compare it with that of healthy children.
Materials and Methods1. Study populationAll children included in the dental examination were patients of the Departments of Pediatrics, Oncology and Hematology, Clinical Hospital No. 4 of the Medical University of Lodz. All were included in a program for the assessment of the late side effects of anticancer treatment in survivors of childhood cancers. Dental examination was performed in the Department of Pediatrics and Orthodontics of the Institute of Dentistry, Medical University of Lodz.
From July 2012 to July 2015, 116 patients were invited for dental examination and 79 of them underwent dental examinations. Six participants were excluded from the panoramic radiography examination: four did not receive parental consent and two others were too young (2 and 3 years). Of those who completed the examination, eight radiographs were disqualified as the patients suffered from oligodontia and they lacked most of teeth in the mandible. A further six patients were also excluded from the investigation as they were aged above 16. Therefore, a total number of 59 patients finally underwent examination: 16 (27.1%) girls and 43 (72.8%) boys.
The children in the study group had been treated for acute lymphoblastic leukemia, acute non-lymphoblastic leukemia, B-cell non-Hodgkin lymphoma, Hodgkin lymphoma, brain tumor, Wilms tumor, hepatoblastoma, neuroblastoma or germinal tumor and rhabdomyosarcoma. For further comparisons, they were divided into subgroups as follows: leukemia, lymphoma, brain tumors, Wilms tumor, hepatoblastoma, neuroblastoma. The remaining eight patients (one patient with germinal tumor and seven with rhabdomyosarcoma) were included in one group named other solid tumors (Table 1).
At the time of the examination, the patients were aged above four and below 16 years (range, 56 to 182 months). At the beginning of anticancer therapy, the youngest child was 1-month-old, and the oldest was 124 months. The mean duration of anticancer therapy was 16.8 months (range, 1 to 47 months), and the mean length of time since the termination of disease was 4.6 years (range, 8 to 123 months). Further clinical details are given in Table 2.
The control group consisted of healthy patients at the Institute of Dentistry of similar ages, i.e., between 4 and 16 years (range, 56 to 191 months), who had been examined by panoramic radiograph in 2013. Of these 582 panoramic radiographs, 38 were rejected due to the presence of a cleft lip or palate, 32 for other congenital disorders, and 40 which had been performed on cancer patients. Finally, 472 radiographs were approved for examination: 228 were taken from patients of the Orthodontics Department and the remaining 244 of the Pediatric Department, Institute of Dentistry. To replace the pantomographs of the older patients from 2013, 30 more were randomly selected from children previously treated in the Pediatrics Department in 2014: all were between the ages of 6 and 8 years. The three most closely-related control subjects with regard to propensity score were matched to each cancer patient. This process resulted in the creation of a sex- and age-matched control group of 177 individuals.
2. DA estimationThe DA in children was estimated according to Demirjian et al. [7]. Briefly, seven left tooth germs in the mandible are assessed radiographically, and then evaluated on a scale based on an eight-stage model of tooth development: initial calcification, fusion of the calcified points, formation of enamel and dentine, formation of crown and radicular bifurcation, elongation of roots and closure of the root apices (Fig. 1). As well as being labelled with the letters A to H, each stage is thoroughly described and awarded a number value, and the eighth numbers are added to give an overall score for the dentition. The final DA of the child can then be estimated by matching the final value in tables prepared separately for girls and boys.
To allow further comparison between the DAs of the two groups, the delta DA for each child was calculated by subtracting his or her chronological age (CA) from the DA: i.e., delta DA=dental age (DA)–chronological age (CA).
The analysis was made twice in 1-month time-interval, by two independent operators (PP and WM) with original interand intraobserver variability 97% and 99%, respectively. Any observed discrepancy was discussed till agreement achieved.
In the group of cancer survivors, the presence of dental anomalies was estimated. Hypodontia was recognized when a tooth germ was missing, microdontia when a tooth was half or less of the size of a comparable homolog [8], and root shortage if the root/crown length ratio was lower than 1.6 (according to a simplified Hölttä Defect Index); [9].
3. Statistical evaluationContinuous variables are presented as means with standard deviations, while nominal variables are presented as numbers followed by percentages in brackets. The ShapiroWilk test was used to assess the normality of distribution. Continuous variables were compared using the Mann-Whitney U test, Wilcoxon and Kruskal-Wallis ANOVA in the case of a non-normal distribution, or the t test in the case of a normal distribution. The Statistica 12.5 PL package (Statsoft, Tulsa, OK) was used for the analysis. p < 0.05 were considered statistically significant. The patients were ranked according to propensity scores calculated using logistic regression corresponding to the probability of being in cancer or control groups, with age and sex being taken into account. Following this, a sex- and age-matched group of healthy individuals was created by matching three controls with the most similar propensity scores to each patient with cancer.
ResultsAmong the cancer patients, 20 children (33.8%) demonstrated the same DA as CA; however, the DA was accelerated for more than 1 month in 25 (42.3%), and delayed by more than 1 month in 14 (23.7%). Among the healthy patients, 69 (38.9%) demonstrated identical DA and CA, while DA was accelerated in 61 (34.4%) and delayed in 47 (26.5%).
Mean DA was accelerated compared to CA in both study groups. However, DA was accelerated by almost 12 months in cancer patients, compared to over six months in controls (Table 2). Cancer survivors also demonstrated a significantly greater acceleration of DA compared with healthy individuals (p=0.04) (Fig. 2).
Children with all types of cancer, besides hepatoblastoma, showed advanced DA, and in most cases, the difference was significant (Table 1). Mean values and standard deviation of delta DA to CA in patients with all cancer types are also illustrated in Fig. 3A. The greatest delta DA, i.e., DA–CA, was observed in the group of patients suffering from brain tumors.
Interestingly, the lowest DA values were noted in patients with hepatoblastoma (HP); in addition, they demonstrated a lower delta DA to CA than patients with other cancer types (p=0.011) and healthy individuals (p=0.037) (Fig. 3B). Four male participants suffered from hepatoblastoma: their detailed clinical features are presented in Table 3. All the HP patients suffered from familial adenomatous polyposis (FAP), three of whom were identified with the adenomatous polyposis coli (APC) genes mutation.
Several clinical characteristics were investigated which may interfere with the dental development of cancer patients. Girls were more advanced in their DA than boys, but the difference was not statistically significant. Previous radiotherapy, radiotherapy of the head or neck, or hematopoietic stem cell transplantation (HSCT) did not appear to have a significant influence on the DA of cancer patients, and neither did anticancer treatment with cyclophosphamide (Table 4). Neither age at diagnosis or termination of disease, nor the length of the treatment significantly influenced DA (data not shown).
In the cancer group, 15 (25.4%) patients had teeth with short roots, 18 (30.5%) had microdontic teeth, and 16 (27.1%) had hypodontia (Table 4).
The cancer patients displaying teeth with short roots were found to be older than those without (p=0.007) and their DA was more advanced (p < 0.001). Their DA was also significantly advanced in relation to their CA (p < 0.001) (Table 4, Fig. 4A). No such relationships were noted in patients with microdontia (Table 4, Fig. 4B).
DiscussionIn our study we found that children treated from cancer have different DA as compared to healthy population. We divided our group according to frequent cancer type showing that majority of patients have accelerated DA. Moreover, we also documented that subgroup of patients with HP, who had delayed DA, might differ from other cancer groups and healthy individuals. Since we performed analysis in many subgroups our approach might be underpowered and needs to be confirmed in the future in larger sample size. However few studies examine changes in DA in cancer survivors, and the available results are confounding. Martin et al. found that in a group of 73 patients treated for leukemia, 56.9% demonstrated normal DA, 11.1% delayed DA and 38.9% accelerated DA [10]. Elsewhere, 40 children who underwent allogeneic HSCT were found to display a higher mean DA than CA [11]. In another study on 50 children treated for various cancers, 37.03% of boys and 52.17% of girls demonstrated a DA that was accelerated by more than five months compared to CA [12].
In the present study, using the Demirjian’s scale, the DA of healthy children was overestimated by approximately 6 months. Other studies have also found DA to be overestimated or underestimated by different scales, and hence employed regression equations adapted to the population studied [13-15]. However, the present study compares two sex- and age-matched groups from the same Caucasian population, which should be subject to the same potential bias.
Despite the development of different scales and methods, the Demirjian’s scale is still considered to be one of most reliable bases for estimating DA in Caucasian children [16]. However, it has been found that in some populations, the scale tends to overestimate DA in relation to the chronological maturity of the child [17,18]. In addition, differences in DA have been found in various populations and these have been attributed to differences in the timing of their overall maturation; for example, a study population of Hong Kong residents were found to be more advanced overall in dental development compared with a British Caucasian population, by an average of 5 months [19].
It has already been proven that DA could be an indicator of CA and that variables such as body mass index could influence dental maturation and terms of tooth eruption [12,20]. Other studies have found positive correlations between DA and CA, and between dental and skeletal ages [21]. During puberty, typically occurring at the age of 8-13 years in girls and 10-15 years in boys, a growth spurt stage takes place, and this is accompanied by the accelerated development of teeth, dental bones, and the skeleton as a whole [21,22]. As girls tend to start their pubertal growth spurt earlier than boys, they tend to demonstrate more advanced mineralization of tooth tissues and earlier dental maturation [12]. This was partially reflected in our study, as girls tended to show more advanced DA than the boys; however, the differences were not significant.
Although dental development typically occurs together with overall physical development, this can be altered in a child by changes in nutrition status and weight [23]. Overweight children have been found to demonstrate more advanced dental development than those with normal or decreased weight [20], while pre-term born children with low or very low birth weight demonstrate delayed tooth development at later ages [24]. However, as body mass can change quickly with the stage of the disease and its treatment, it can be difficult to use patient weight as an indicator of development in children with cancer.
In our study, patients wih HP demonstrated significantly delayed dental development compared to other patients. According to the medical records, all four HP patients suffered from FAP and three of them had documented APC genes mutations. Such associations between HP, APC genes mutation and FAP have already been documented in previous papers [25]. However, FAP and cleidocranial dysplasia are regarded as two of the most commonly-associated syndromes connected with supernumerary teeth [26]. Moreover, APC mutation is known to be responsible for so-called Gardner’s syndrome, in which patients suffer from FAP, sebaceous cysts, jaw osteomas, supernumerary teeth, and delayed tooth eruption [27]. None of our HP patients presented supernumerary teeth, and none missed any tooth germs, but one was found to have a tooth with short roots and another with four microdontic teeth.
Within the cancer group, 15 patients demonstrated teeth with short roots (SR), and had chronological and DAs that were significantly higher than of the other 44. Such a situation is unavoidable as SR can be identified only in older children, in which the processes of tooth root elongation and apex closure have already finished. However, significant differences were found between the two groups, i.e., those with and those without SR, with regard to delta DA to CA. Suggesting that cancer patients with SR were at more advanced stages of tooth development than the others, nevertheless their CA. It is in accordance with results gained by other authors, who found that the agents, especially the cyclophosphamide, used during the cancer therapy might be responsible for the premature closure of the tooth apices [4]. It should be stressed that the treatment regimen of HP patients does not include cyclophosphamide.
The cancer group also included 18 patients with microdontic teeth, which DA did not differ from that of the patients without such an anomaly.
Our findings indicate that of the cancer patients, 16 who suffered from hypodontia were younger and had a lower DA than the remaining 43. This supports the previous findings that younger children are more likely to suffer from more severe complications like hypo- or oligodontia [3,8]. It has also been found that DA tends to be delayed in healthy patients with dental agenesis [28]. Although the agenesis of teeth is typically due to gene mutations, it might be also influenced by anticancer therapy [3,8]. The observed lack of significance could be also partially explained by the fact that patients with oligodontia, i.e., those missing more than six tooth germs, were excluded at the beginning of the investigation.
The DA of cancer patients differs from that of healthy children at the same CA.
NotesEthical Statement The study was approved by the Ethical Committee of the Medical University of Lodz (IRB number: RNN/37/13/KE). Written informed consent for dental and panoramic examinations was obtained from both parents, or from guardians and patients for those above the age of 16. Fig. 1.Diagram of Demirjian’s classification. Stage description (Demirjian et al. Hum Biol. 1973;45:211-27 [7]). (A) In both radicular and multiradicular teeth, a beginning of calcification is seen at the superior level of the crypt in the form of an inverted cone or cones. There is no fusion of these calcified points. (B) Fusion of the calcified points forms one or several cusps which unite to give a regularly outlined occlusal surface. (C) Enamel formation is complete at the occlusal surface. Its extension and convergence towards the cervical region is seen. The beginning of a dentinal deposit is seen. The outline of the pulp chamber has a curved shape at the occlusal border. (D) The crown formations completed down to the cemento-enamel junction. The superior border of the pulp chamber in the uniradicular teeth has a definite curved form, being concave towards the cervical region. The projection of the pulp horns if present, gives an outline shaped like an umbrella top. In molars the pulp chamber has a trapezoidal form. Beginning of root formation is seen in the form of a spicule. (E) Uniradicular teeth: The walls of the pulp chamber now form straight lines, whose continuity is broken by the presence of the pulp horn, which is larger than in the previous stage. The root length is less than the crown height. Molars: Initial formation of the radicular bifurcation is seen in the form of either a calcified point or a semi-lunar shape. The root length is still less than the crown height. (F) Uniradicular teeth: The walls of the pulp chamber now form a more or less isosceles triangle. The apex ends in a funnel shape. The root length is equal to or greater than the crown height. Molars: The calcified region of the bifurcation has developed further down from its semi-lunar stage to give the roots a more definite and distinct outline with funnel shaped endings. The roots length is equal to or greater than the crow height. (G) The walls of the root canal are now parallel and its apical end is still partially open (distal root in molars). (H) The apical end of the root canal is completely closed (distal root in molars). The periodontal membrane has a uniform width around the root and the apex. 
Fig. 2.Differences in dental age to chronological age between cancer survivors and control patients. 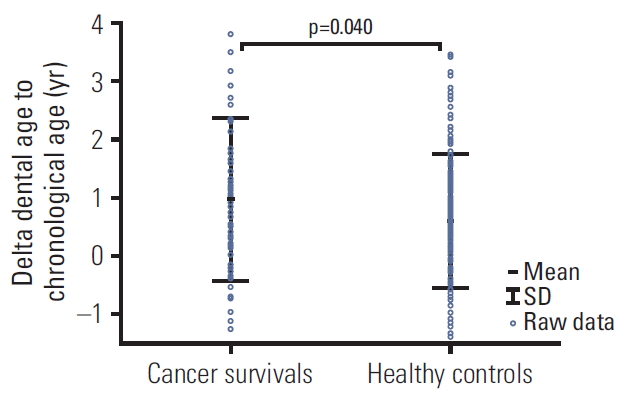
Fig. 3.Values of delta dental age to chronological age in patients with different types of cancer (A) and hepatoblastoma compared to the healthy patients and other cancer patients (B). Gray zone represents interquartile range for healthy controls. 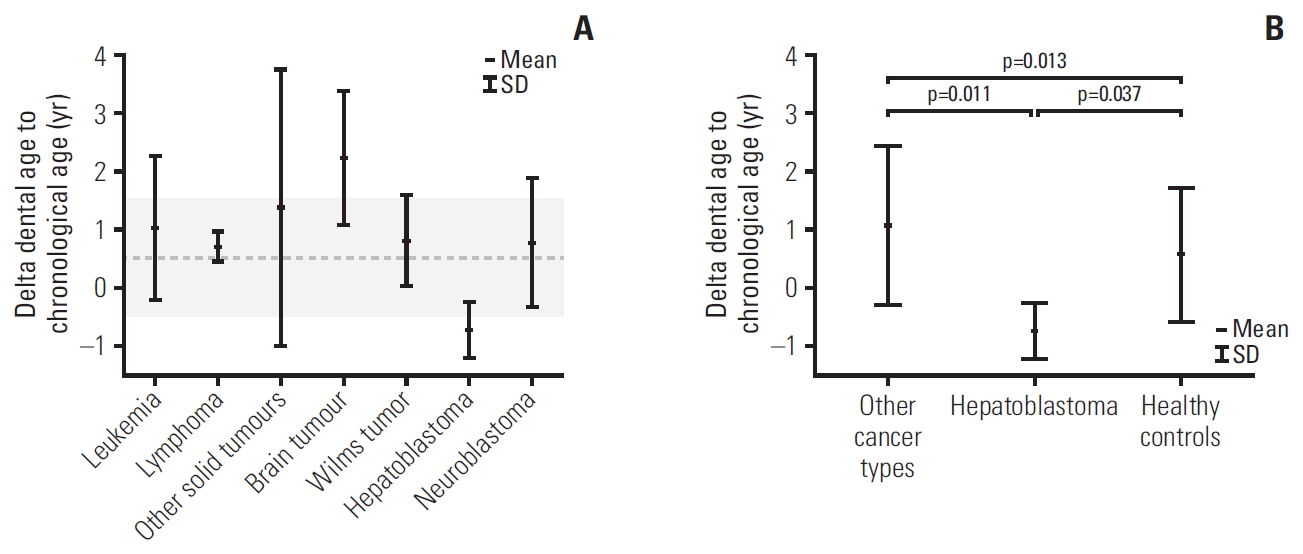
Fig. 4.Differences in dental age to chronological age in cancer patients according to tooth abnormalities: short roots (A), microdontic teeth (B), and hypodontia (C). 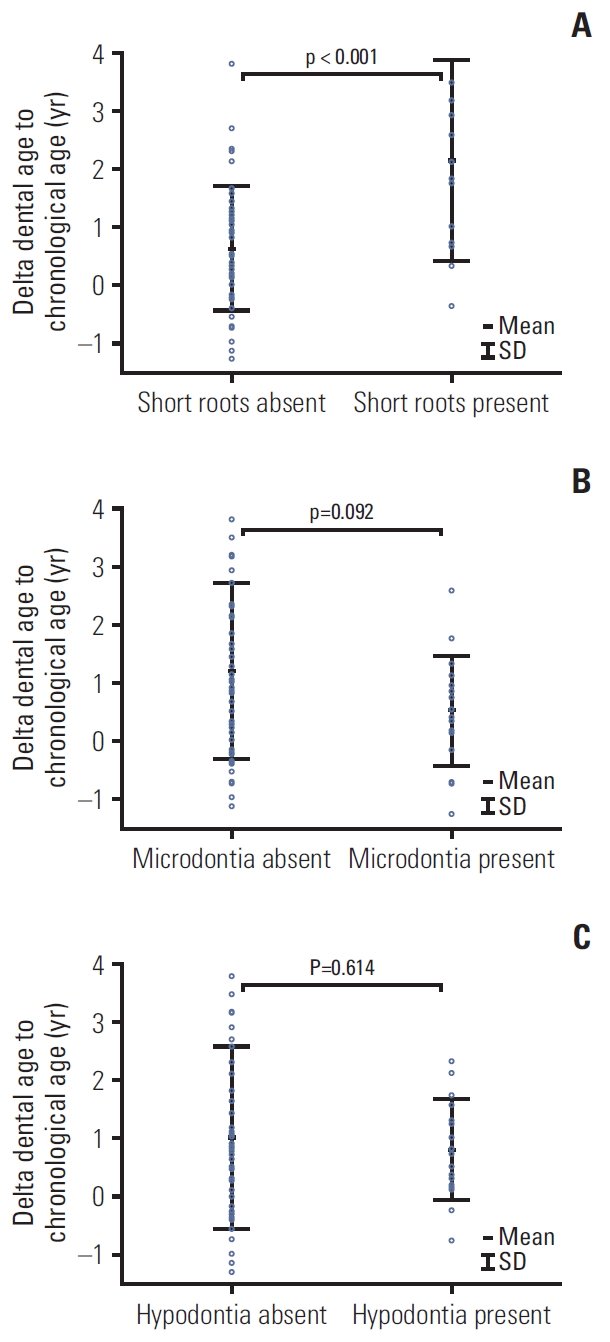
Table 1.Types of cancer in examined patients
Table 2.Differences in chronological and dental ages between study and healthy age- and sex-matched control groups Table 3.Clinical characteristics of four patients suffered from hepatoblastoma Table 4.Chronological and dental age in different groups of cancer patients References1. Zubowska M, Wyka K, Fendler W, Mlynarski W, Zalewska-Szewczyk B. Interleukin 18 as a marker of chronic nephropathy in children after anticancer treatment. Dis Markers. 2013;35:811–8.
2. Kang CM, Hahn SM, Kim HS, Lyu CJ, Lee JH, Lee J, et al. Clinical risk factors influencing dental developmental disturbances in childhood cancer survivors. Cancer Res Treat. 2018;50:926–35.
3. Proc P, Szczepanska J, Skiba A, Zubowska M, Fendler W, Mlynarski W. Dental anomalies as late sdverse rffect among young children treated for cancer. Cancer Res Treat. 2016;48:658–67.
4. Kawakami T, Nakamura Y, Karibe H. Cyclophosphamide-induced morphological changes in dental root development of ICR mice. PLoS One. 2015;10:e0133256
5. Kaste SC, Goodman P, Leisenring W, Stovall M, Hayashi RJ, Yeazel M, et al. Impact of radiation and chemotherapy on risk of dental abnormalities: a report from the Childhood Cancer Survivor Study. Cancer. 2009;115:5817–27.
6. Avery JK, Steele PF, Avery N. Oral development and histology. 3rd ed. Stuttgart: Thieme; 2002.
7. Demirjian A, Goldstein H, Tanner JM. A new system of dental age assessment. Hum Biol. 1973;45:211–27.
8. Holtta P, Alaluusua S, Saarinen-Pihkala UM, Peltola J, Hovi L. Agenesis and microdontia of permanent teeth as late adverse effects after stem cell transplantation in young children. Cancer. 2005;103:181–90.
9. Holtta P, Hovi L, Saarinen-Pihkala UM, Peltola J, Alaluusua S. Disturbed root development of permanent teeth after pediatric stem cell transplantation. Dental root development after SCT. Cancer. 2005;103:1484–93.
10. Martin MB, Li CS, Rowland CC, Howard SC, Kaste SC. Correlation of bone age, dental age, and chronological age in survivors of childhood acute lymphoblastic leukaemia. Int J Paediatr Dent. 2008;18:217–23.
11. van der Pas-van Voskuilen IG, Veerkamp JS, Raber-Durlacher JE, Bresters D, van Wijk AJ, Barasch A, et al. Long-term adverse effects of hematopoietic stem cell transplantation on dental development in children. Support Care Cancer. 2009;17:1169–75.
12. Flores AP, Monti CF, Brunotto M. Dental and chronological age in children under oncological treatment. J Forensic Sci. 2015;60:453–6.
13. Tomas LF, Monico LS, Tomas I, Varela-Patino P, Martin-Biedma B. The accuracy of estimating chronological age from Demirjian and Nolla methods in a Portuguese and Spanish sample. BMC Oral Health. 2014;14:160.
14. Rozylo-Kalinowska I, Kiworkowa-Raczkowska E, Kalinowski P. Dental age in Central Poland. Forensic Sci Int. 2008;174:207–16.
15. Sobieska E, Fester A, Nieborak M, Zadurska M. Assessment of the dental age of children in the Polish population with comparison of the Demirjian and the Willems methods. Med Sci Monit. 2018;24:8315–21.
16. Chudasama PN, Roberts GJ, Lucas VS. Dental age assessment (DAA): a study of a Caucasian population at the 13 year threshold. J Forensic Leg Med. 2012;19:22–8.
17. Esan TA, Schepartz LA. The timing of permanent tooth development in a Black Southern African population using the Demirjian method. Int J Legal Med. 2019;133:257–68.
18. Wang J, Bai X, Wang M, Zhou Z, Bian X, Qiu C, et al. Applicability and accuracy of Demirjian and Willems methods in a population of Eastern Chinese subadults. Forensic Sci Int. 2018;292:90–6.
19. Jayaraman J, Roberts GJ. Comparison of dental maturation in Hong Kong Chinese and United Kingdom Caucasian populations. Forensic Sci Int. 2018;292:61–70.
20. Chehab DA, Tanbonliong T, Peyser J, Udin R. Association between body mass index and dental age in Hispanic children. Gen Dent. 2017;65:54–8.
21. Hashim HA, Mansoor H, Mohamed MH. Assessment of skeletal age using hand-wrist radiographs following Bjork system. J Int Soc Prev Community Dent. 2018;8:482–7.
22. Ferrandez A, Carrascosa A, Audi L, Baguer L, Rueda C, Bosch-Castane J, et al. Longitudinal pubertal growth according to age at pubertal growth spurt onset: data from a Spanish study including 458 children (223 boys and 235 girls). J Pediatr Endocrinol Metab. 2009;22:715–26.
23. Brinksma A, Roodbol PF, Sulkers E, Kamps WA, de Bont ES, Boot AM, et al. Changes in nutritional status in childhood cancer patients: a prospective cohort study. Clin Nutr. 2015;34:66–73.
24. Paulsson L, Arvini S, Bergstrom N, Klingberg G, Lindh C. The impact of premature birth on dental maturation in the permanent dentition. Clin Oral Investig. 2019;23:855–61.
25. Giardiello FM, Petersen GM, Brensinger JD, Luce MC, Cayouette MC, Bacon J, et al. Hepatoblastoma and APC gene mutation in familial adenomatous polyposis. Gut. 1996;39:867–9.
26. Lubinsky M, Kantaputra PN. Syndromes with supernumerary teeth. Am J Med Genet A. 2016;170:2611–6.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||